Community Conversations
July 2021
This Community Conversations post is part of a series highlighting our Community Advisory Board members and the work they do in the community…
 My name is Tommy Dennis. I have been a member of the Great Plains IDeA-CTR Community Advisory Board since March of 2021. I was asked to join the advisory board due to my work with marginalized communities. I am currently employed at the Nebraska AIDS Project as their Outreach Coordinator, where I specifically work to engage and educate individuals who identify as Black, Gay and Bisexual men (BGBM).
My name is Tommy Dennis. I have been a member of the Great Plains IDeA-CTR Community Advisory Board since March of 2021. I was asked to join the advisory board due to my work with marginalized communities. I am currently employed at the Nebraska AIDS Project as their Outreach Coordinator, where I specifically work to engage and educate individuals who identify as Black, Gay and Bisexual men (BGBM).
My work specifically focuses on the BGBM community and improving their access to testing, prevention and for those already diagnosed as living with HIV, Linkage to Care. Nebraska AIDS Project (NAP) not only focuses on prevention services but also improving the health outcomes of those living with HIV and AIDS. We also provide access to preventative methods such as free contraceptives and PrEP (Pre-exposure prophylaxis) which is a once a day medication to prevent the transmission of HIV. Additionally, NAP is the only statewide AIDS Service Organization, servicing Omaha, Lincoln, Norfolk, Scottsbluff and Kearney. Additionally, we also serve portions of Southwest Iowa and Wyoming. Evidence has shown the social determinants play a major role in overall health outcomes of People Living with HIV (PLWHIV). We at the Nebraska AIDS Project strive to reduce as many of those barriers as possible. Specifically with housing, food insecurity, and transportation.
My specific targeted outreach is geared towards priority populations and strives to meet individuals where they are at in an effort for them to learn their status. This oftentimes includes partnering with various community entities such as churches, drug rehabilitation facilities, and even the Department of Corrections. These are locations where we have been able to best engage our priority populations in the most meaningful way that we can.
June 2021

About the author: Thayne Munce, PhD, FACSM is the Director of the Athletic Health & Performance Lab and an Assistant Scientist in the Environmental Influences on Health and Disease Group at Sanford Research (Sanford Health) and is also an Associate Professor in the Department of Pediatrics at the University of South Dakota Sanford School of Medicine.
Football is beloved by millions of fans in the United States and is one of the most popular youth and high school sports in the country. Over the past two decades, new information about brain injuries in football players has raised serious concerns about the safety of this sport. While most of the alarming data have come from retired professional football players, numerous questions about the risks to younger players have recently emerged. From a public health perspective, this makes sense, as approximately 95% of all tackle football players in the US are high school-age or younger. Furthermore, there are additional concerns about the effects of concussions and repetitive head impacts on the developing brains of children and adolescents.
In response, flag football has been promoted as a safer alternative to tackle football. In addition to the lower perceived injury risk, flag football players are thought to be more active during play, which could result in greater health benefits. While these assumptions are reasonable, there is very little data to support or refute them. Determining the relative risks and benefits of youth tackle and flag football would be important to help guide public policy in an evidence-based manner and to help parents and their children make informed decisions about their own participation.
Since 2011, my research team has been studying health and safety issues in youth football. This work has evolved into the First Down Project, with a mission dedicated to improving the health, safety and performance of football players through innovative, high-impact research. In 2020, I received a Great Plains IDeA-CTR Pilot Grant to address questions about the comparative risks and benefits of youth tackle and flag football. The title of this specific project is “Injury Rates and Physical Activity in Youth Football: Tackle vs. Flag”. This work is being conducted in partnership with South Dakota Junior Football, Inc, a community-based youth football organization that offers tackle and flag football leagues of overlapping ages. This league structure provides an ideal setting to evaluate injury rates and physical activity between youth tackle and flag football players from the same community.
Despite a shortened season due to the COVID pandemic, we were able to measure the physical activity of a limited number of tackle and flag football players last year. Players on two tackle teams and two flag teams wore small GPS monitors during all practices throughout the season. In addition, the tackle players wore their GPS monitors during games (flag games were played indoors where the GPS monitors were inoperable). GPS monitoring allowed us to measure several indices of physical activity including total distance covered, distance while walking, jogging, or sprinting, work rate (distance / time), and walking/running speed. While we are still analyzing these preliminary data, it is apparent that there are indeed differences in several physical activity characteristics between youth tackle and flag football players.
Through this study and the broader work of our First Down Project, we will continue to pursue the answers to meaningful research questions focused on the health and safety of youth football players. Specifically, we want to generate and share new information so that parents and their children can make educated decisions to minimize their risks and maximize their benefits of football participation.
If you have any questions about this research, please contact me at thayne.munce@sanfordhealth.org.
May 2021
Understanding COVID-19 in North Omaha: A Brief Community Assessment
The North Omaha Community Care Council (NOCCC) is a 501(c)3 non-profit organization comprised of health, education, faith-based, and local government agencies who work together to improve communication, access to affordable and quality health care, education, information, and disseminate helpful resources and services to the North Omaha community. Through a partnership with Clair Memorial United Methodist Church, University of Nebraska Medical Center-Center for Reducing Health Disparities and College of Nursing, and North Omaha Area Health (NOAH) Clinic, the NOCCC conducted a brief assessment to identify the needs and understand knowledge and behaviors related to COVID-19 in North Omaha.
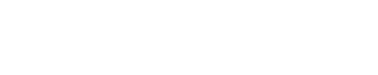
The brief assessment consisted of questions about COVID-19 safety practices (e.g., wearing a mask), frequent source of information about COVID-19, unmet basic need during the pandemic, and demographic information. The assessment was administered at Clair Memorial United Methodist Church from September to November 2020 to North Omaha residents.
Findings
 We collected 582 assessments, only 18 away from our goal of 600 assessments. Most of the residents who completed the assessment were Black women, with a relatively even distribution across age categories (11.25% of residents in each age category). Below we highlight some of the most important findings:
We collected 582 assessments, only 18 away from our goal of 600 assessments. Most of the residents who completed the assessment were Black women, with a relatively even distribution across age categories (11.25% of residents in each age category). Below we highlight some of the most important findings:
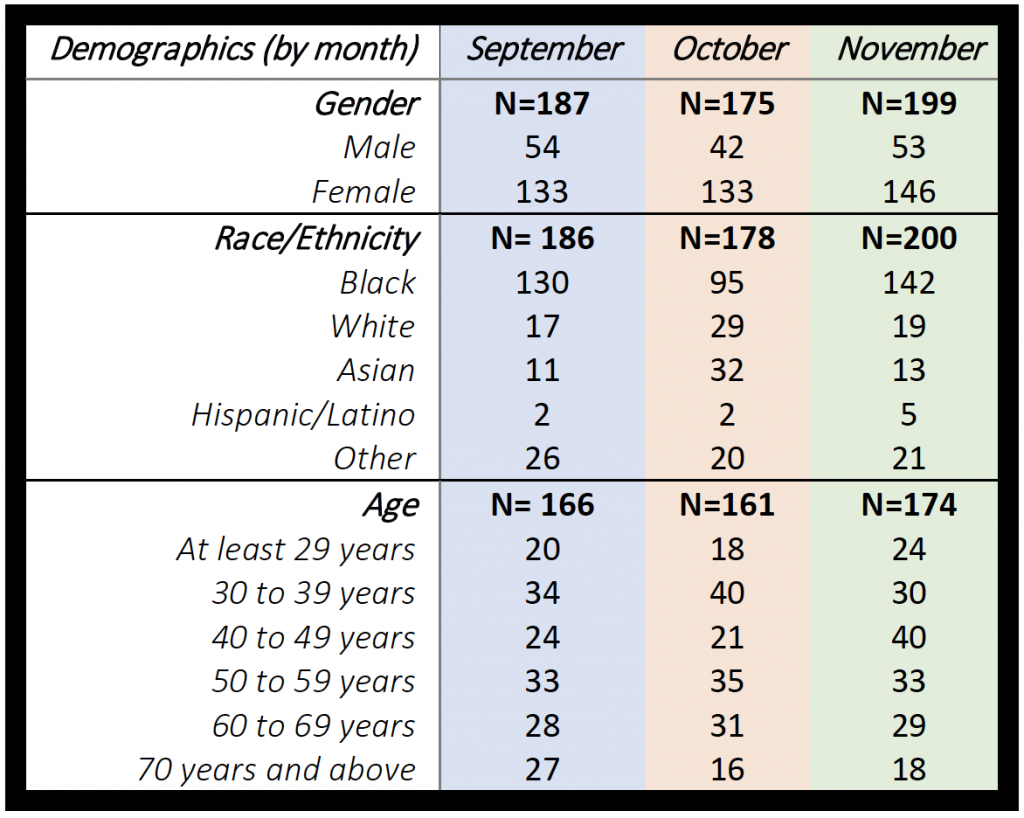
- Unemployment rate decreased from 58% in September to 46% in November. However, the percentage of North Omaha residents who lost their jobs due to the COVD-19 pandemic increased from 27% in September to 33% in November.
- Groceries, health of family members, and personal health concernswere the top three stressors during the pandemic.
- The number of North Omaha residents who reported wearing face coverings/masks daily increased from 89% in September to 95% in November. Social distancing also increasedfrom 85% in September to 96% in November.
- More than 40% of North Omaha residents believed they could get sick from COVID-19 from September to November. However, only residents in the age categories 40 to 49 years and 70 years and above expressed the highest level of COVID-19 infection concerns (79% for each age category).
- Data on COVID-19 infection were not collected in September. However, a question was added in the October and November assessments in which 3% of the North Omaha residents reported they had COVID-19 in October. Of those 3%, approximately 1% reported being asymptomatic, and 2% reported being ill due to the virus. In November, 5% of residents reported contracting the virus. Among these residents, 1% reported being asymptomatic, and 4% reported being ill.
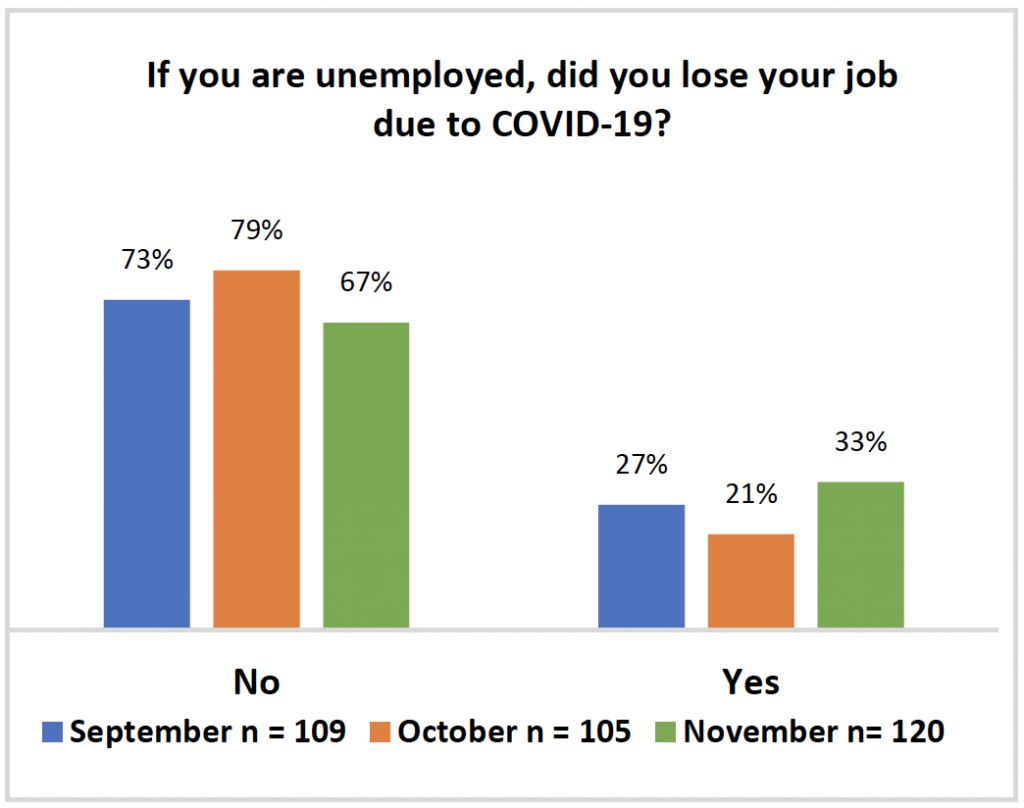
- Most North Omaha residents reported their main source for information and education on COVID-19 coming from the news and their health care provider.
 In light of these findings, there are several important actions that must take place. First, it is important that we leverage these types of data to mobilize various community residents, partners, and other entities to swiftly and equitably approach the contextual effects of COVID-19 in North Omaha. While we are working to vaccinate Nebraskans, it is important to think about how we can provide support for social factors such as food, housing, employment, health (physical and mental), and education, among others. We must continue to ensure community residents are properly educated about COVID-19, the vaccines, and the importance of continuing safety practices while our local government and non-government officials work to get Nebraskans fully vaccinated. It is also critical to understand how residents get their information and to use this knowledge to distribute information effectively. Lastly, ensuring that North Omaha residents have equitable access to the vaccine is also crucial to prevent more people being affected by COVID-19.
In light of these findings, there are several important actions that must take place. First, it is important that we leverage these types of data to mobilize various community residents, partners, and other entities to swiftly and equitably approach the contextual effects of COVID-19 in North Omaha. While we are working to vaccinate Nebraskans, it is important to think about how we can provide support for social factors such as food, housing, employment, health (physical and mental), and education, among others. We must continue to ensure community residents are properly educated about COVID-19, the vaccines, and the importance of continuing safety practices while our local government and non-government officials work to get Nebraskans fully vaccinated. It is also critical to understand how residents get their information and to use this knowledge to distribute information effectively. Lastly, ensuring that North Omaha residents have equitable access to the vaccine is also crucial to prevent more people being affected by COVID-19.
April 2021

This Community Conversations post is part of a series highlighting our Community Advisory Board members and the work they do in the community…
My name is Amy Behnke and I have been a member of the Great Plains IDeA-CTR Community Advisory Board since its inception. I was asked to serve on the CAB because my day-to-day work focuses on ensuring underserved and marginalized populations have access to health care, regardless of insurance status or ability to pay.
In my role as the CEO of the Health Center Association of Nebraska (HCAN), I work with Nebraska’s seven Federally Qualified Health Centers (FQHCs). HCAN is dedicated to supporting the health centers and the patients they serve through training, technical assistance, collaborative partnerships and advocacy. We believe that everyone deserves access to high quality health care, and that health centers play a key role in ensuring equitable access to that care. These health centers provide primary medical, dental and behavioral health services to over 115,000 Nebraskans across the state. They also support their patients through enabling services like translation, transportation and outreach and enrollment services.
The majority of health center patients are low income and of a racial or ethnic minority, and nearly half are uninsured. Their health care needs aren’t limited to the care they receive inside the four walls of the health centers. Environmental factors, stable housing, economic instability and food security are just a few of the social factors that can disrupt health outcomes. I believe that the CAB is a critical collaboration whose goals and resulting research opportunities will help us better understand those health disrupters and truly address community health needs.
March 2021

Obesity is one of our Community Advisory Board’s identified regional health priorities due to the high prevalence in the Great Plains, and disparities in prevalence and outcomes for under-represented minority populations and people living in rural areas. Addressing obesity early, either through prevention or treatment of childhood obesity, has the potential to prevent a lot of chronic health conditions and expenses later in life. So, over the past year we formed a workgroup with Children’s Hospital and Medical Center, members of the Great Plains IDeA Clinical and Translational Research Network, and the Child Health Research institute to talk about childhood obesity. We started with a mindset to understand how pediatricians and healthcare administrators, when partnered with researchers, could have a significant impact on preventing and reducing childhood obesity.
After a few meetings the group came up with the following short-, mid-, and long-term goals to:
- Develop a sustainable workgroup of healthcare administrators, providers, scientists, and facilitators focused on childhood obesity prevention and treatment across organizations to advance science while concurrently improving childhood obesity-related practice in Nebraska.
- Test methods to facilitate the implementation of childhood obesity research that aligns with current practice needs.
- Conduct pragmatic translational research from basic through population health science.
- Contribute to the successful competition for a national nutritional obesity research center in Nebraska.
- Demonstrate sustained improvements in practice that reduce childhood obesity.
As we move forward with this emerging workgroup, we are focused on being action and project-oriented and providing a place and opportunities for clinical and community partners to work with research partners to develop project ideas that can advance science and improve practice.
We are excited to get this workgroup going and if you are a practitioner or community partner, the benefits of joining the workgroup include: (1) engaging in research that can have direct impact on improving practice, (2) getting support to apply state of the science on obesity prevention and management in your setting, (3) participate in shared projects to build your research capacity, and (4) getting a chance to talk about solutions with researchers and practitioners with similar interests.
Key partners in the workgroup include:
- Child Health Research Institute (Lifespan Disease and Population Health Workgroups)
- City Match
- University of Nebraska at Kearney (Exercise Science/ PA and Wellness Lab)
- University of Nebraska Lincoln (NPOD; Psychology)
- UNMC (Health Promotion; Epidemiology; Pediatrics)
- Children’s Hospital and Medical Center (Pediatrics; Center for the Child and Community)
We are really excited to see what this workgroup brings; and it has even developed some initial metrics of success that include goals to increase the number of inter-disciplinary/inter-professional collaborations, participatory research project, communities involved (especially those that experience disparities), practical scientific advances, and improvements clinical and community practice, policies, and guidelines. If this is something you’d like to get involved in just contact Paul Estabrooks to get on the list!
February 2021
This Community Conversations post is part of a series highlighting our Community Advisory Board members and the work they do in the community…

My name is Susan Mayberger and I have been involved in the Great Plains IDeA-CTR Community Advisory Board (CAB) since the beginning. I was asked to be on the Board because I was the Chair of the South Omaha Community Care Council and because of my work as the Coordinator for the ESL, Migrant and Refugee Education program for the Omaha Public Schools. I was motivated to be part of this Board because I wanted to bring the perspective of the immigrant, migrant and refugee communities in Omaha to the process. Most of the people that I served in my role at OPS had recently arrived and/or didn’t speak English. I had been in this Coordinator position for 19 years and so I was also able to provide a historical perspective to the CAB of these new Americans that were settling in Omaha. I did retire from OPS and am no longer on the Board of the South Omaha Community Care Council but I am now the Chair of the Omaha Refugee Task Force (ORTF) which enables me to continue to provide the perspective of refugees and organizations that support refugees to the CAB process.
ORTF is a network of over 200 individuals and organizations that are committed to the successful integration of refugees and immigrants in our community. ORTF is organized around the areas of health, mental health, education, employment and housing for refugees. Omaha will be resettling increasing numbers of refugees and so the need to include the refugee and immigrant communities in research will also increase. I also hope that ORTF can be part of increasing the diversity of people that go into the health professions. I strongly believe that the goals set out by the CAB are important and through the grant process will bring research that will in the end provide better health outcomes to our community.
January 2021
RFD-TV – media devoted to rural issues, concerns and interests – recently hosted UNMC and UNO Chancellor Jeffrey P. Gold, MD, for their “Rural Health Matters” broadcast. Dr. Gold was joined by Anthony Fauci, MD, Director of the National Institute of Allergy and Infectious Diseases. The topic was the COVID vaccine rollout in the context of rural health. Click the play button above to watch the video.
December 2020

One issue that researchers face is making sure they are recruiting groups of study participants that are representative of the community. Historically, this has been a difficult task and can often end up as a weakness mentioned along with the study results. This is a problem because as science moves forward to benefit all of society, the lack of diversity in studies – especially studies with potentially immediate impact on communities – can lead to an incorrect interpretation of study results or an inability to confirm the potential benefits the study.
This challenge not only affects a researcher’s ability to produce reliable study results, but it also slows the pace of scientific discovery. People who would otherwise benefit from these studies, may have to wait longer to experience these benefits, or may not see them at all. Why does this problem exist? Simply put, the differences in our genes, lifestyle, and environment leads to a difference in our health and our body’s receptiveness to treatment. The National Institute of Health (NIH) understands this challenge. To address this issue, the NIH initiated the “All of Us” Research Program in 2018 with the goal of enrolling a diverse group of at least 1 million people across the United States to accelerate the pace of biomedical research and improve health. The program also aims to make the research results accessible to participants, and it is developing new approaches to generate, access, and make data broadly available to researchers.
The Great Plains IDeA-CTR Network is working with representatives from the “All of Us” program to host a WEBINAR to educate both researchers and community members about the program’s benefits and opportunities. On Monday, January 25th from 11:00 am to noon, speakers will provide an overview of the program, and how researchers can access and use the data to study how factors such as our background, environment, and lifestyle impact why we get sick or stay healthy. This webinar will be followed by a separate webinar specifically tailored to community members and organizations, although if you are interested in participating in the research program then you are encouraged to virtually attend both events. All are welcome! Please see our EVENT CALENDAR for more details on the upcoming webinars. And feel free to EMAIL us with any questions you may have concerning the webinar.
The All of Us Research program provides an opportunity for all communities to be represented in important research projects. It’s time for all communities to be represented in health research! The future of health starts with all of us. Learn how you can help change the future of health by viewing the recorded WEBINAR.
November 2020
Introducing the Community-Engaged Clinical and Translational Research Incubator
Clinical and translational researchers and community partners call for resources to help develop community-engaged research that is competitive for NIH funding.
The Community Engagement and Outreach Core (CEO) of the Great Plains IDeA Clinical and Translational Research Network (GP-IDeA-CTR) is charged with helping to make health research more relevant to communities. To do that we need community partners that are interested in supporting and guiding research.
As the CEO Core, we’ve provided a lot of consultation to researchers on how best to initiate community partnerships that can support their research. Our consultations have included feedback from Core members (Drs. Paul Estabrooks, Keyonna King, Dave Palm, and Heidi Keeler) and from our Community Advisory Board (CAB) made up of representatives from different community-based organizations.
Some of the folks that we have consulted with have been successful getting federal funding for their research. BUT, we think we can do more!
We also received feedback that it would be great to have an opportunity for researchers and their community partners to engage in ongoing consultation starting with the development of the research question and consideration on the degree of community-engagement necessary (e.g., consultation through shared leadership).
Our team has experience in participating in “shared leadership” projects using a community-based participatory research (CBPR) approach. This approach has a goal to conduct research that equitably involves all partners throughout the research process and recognizes the unique strengths of each partner. CBPR is considered a gold standard for community-engaged research.
In our experience, community partners and community organizations interested in expanding their research footprint, and those looking for opportunities to join or develop their own research ideas were interested in: 1) assessing community capacity to conduct research, 2) providing ongoing support to address how best to engage researchers, 3) learning how to effectively and meaningfully work with researchers to develop research studies/proposals that are relevant in their communities, and 4) determining practical but innovative methods.
The Community-Engaged Clinical and Translational Research Incubator will facilitate the development and submission of high-quality and competitive NIH research proposals.
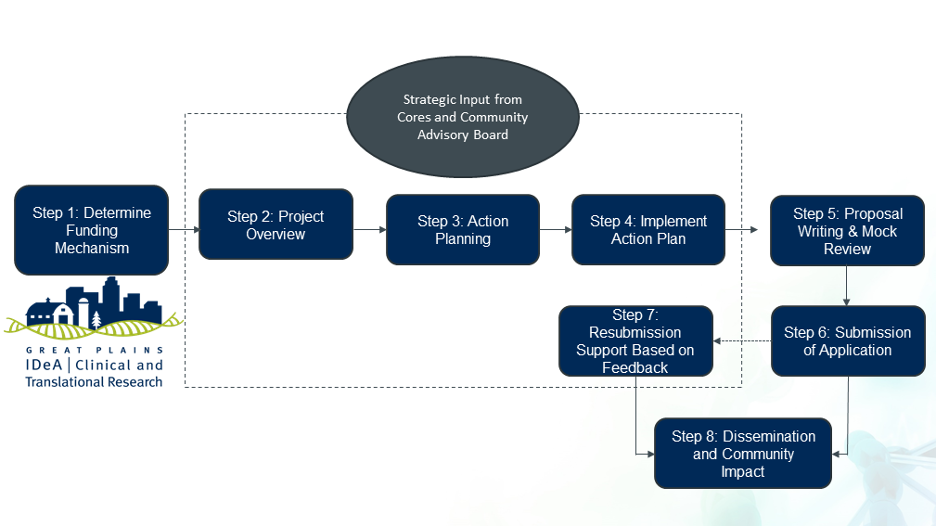
To help community partners and researcher to develop winning proposals and projects, we are introducing the Community-Engaged Research Incubator. It has a lot of moving parts, but we summarized the process in 8 steps (see Figure 1 above). The Incubator is designed to use ongoing scientific and community support, and the strategic participation of other GP-IDeA-CTR Cores (e.g., Professional Development; Biomedical Informatics, Bioinformatics, and Cyberinfrastructure Enhancement; Biostatistics, Epidemiology, and Research Design) depending on the need of each community-engaged research team that participates. The Incubator will focus on developing proposals that can compete for federal grants.
The intended users of the Incubator are GP-IDeA-CTR Members and Community Partners.
Community-engaged CTR teams, which include researchers and community partners that have the potential to develop successful NIH grant applications that provide an impact for partner communities and advance translational science. We anticipate that this resource will benefit both research investigators and community partners.
What are the expectations we have for the Incubator?
We hope that the Incubator will result in short-term outcomes that improve the collaborative capacity of the research team (measured using common community-engaged research metrics), increase the number of community-engaged CTR grant proposals submitted, and lead to higher grant award success rates. In the long-term we hope to demonstrate that research developed as part of the Incubator will demonstrate a meaningful community impact, sustained community partnerships, and the movement of science along the translational spectrum.
How can you access the Community-Engaged CTR Incubator?
Applications will be accepted twice per year, during the first and third quarter of each award year. We will circulate a call for applications in January 2021. An application will include a letter of intent that provides evidence of community engagement , and evidence that the research question addresses a GP-IDeA-CTR priority health area which were established in partnership with the CAB. Applicants will be required to provide a description of how the project will move a scientific idea from one CTR stage to the next (e.g., moving from efficacy to effectiveness) as well as the potential to benefit the community. Finally, the applicant team will outline the potential for federal funding and the partnership’s commitment to participate in a 6- or 12-month incubator that finishes with a grant submission. The CEO Core and CAB will review applications against these criteria and select the top 2-3 applicants per cycle. In addition, proposals that are submitted, but not funded, will also have access to engage the CEO consultation resources to develop a strong resubmission.
October 2020

The annual Berggren Lecture Series is dedicated to Drs. Warren and Gretchen Berggren, long time advocates of public health and primary care approaches to address poverty and infant mortality. The Berggrens both graduated from UNMC in the late 1950s and followed their medical education with advanced degrees in Public Health from Harvard. They spent much of their careers providing medical care for the homeless in Omaha, serving as medical missionaries in the Belgian Congo (later Zaire), and developing voluntary community health worker networks to address health globally in low-income countries. Documented outcomes of their work included improve access to food, quality dietary intake, and decreases in stunted growth patterns common in low-income countries as well as developing strong health care and community partnerships that eradicated tetanus in a region in Haiti where 1 in 3 children were affected, historically, by tetanus.
The purpose of The Berggren Lecture Series is to honor the legacy of Drs. Gretchen and Warren Berggren by highlighting current partnerships between public health professionals and clinical and community organizations that (1) address the most pressing public health issues of our time, (2) study methods to move evidence for health promotion, disease prevention, and public health into typical community settings, and (3) move science forward while documenting community improvements in health and well-being.
This year, the lecture series was held virtually and featured presentations from local medical and public health experts as well as Dr. Ruth Berggren, Professor of Medicine – Infectious Disease at UT Health in San Antonio, the Director of the Center for Medical Humanities and Ethics, and daughter of Warren and Gretchen Berggren. Ruth discussed her experience caring for patients and populations in the wake of disasters and provides lessons learned in the aftermaths of recent disasters such as Hurricane Katrina, the Haiti Earthquake, and the COVID-19 pandemic. Other presenters described the importance of crisis communication, the concept of health equity and how the COVID-19 pandemic has affected health disparities in minority communities, and how we honor the legacy of the Berggrens by exploring ethical solutions to public health and primary care issues. Find and watch all the 2020 Berggren Series lectures on the UNMC College of Public Health Department of Health Promotion website.
September 2020
Conducting community-engaged research is challenging. In the midst of a pandemic, it can seem impossible. The second meeting of our Community-Engaged Research Interest Group (CEnRIG) gave us insight into the obstacles community-engaged researchers and their partners are facing including the changes experienced in different research areas and how some investigators have overcome these challenges. The purpose was to address important questions in the time of COVID-19: What do communities need from researchers right now? How can we overcome tech-related barriers with our research partners and participants? And, of course, what have been the biggest “Aha!” moments while conducting research in this pandemic? This discussion was paneled by two academic researchers and a community leader with years of experience in building partnerships. Alice Ammerman, DrPh, is a professor in the Department of Nutrition at the Gillings School of Global Public Health, and the Director of the Center for Health Promotion and Disease Prevention at UNC-Chapel Hill. Risto Rautiainen, PhD, is a Professor in the Department of Environmental, Agricultural & Occupational Health in the College of Public Health at UNMC. Doris Lassiter is the president and CEO of Doris Lassiter Consulting, LLC and has worked to address health disparities for decades, establishing programs and initiatives to lessen the burden on minority health. Some of the main takeaways from the session are great advice for folks hoping to continue their work and their relationships with communities. For instance,- Right now might not be the best time to start a new partnership; investigators should look towards formed partnerships for the time being.
- Involving the community at all stages of the project from start to finish is more important than ever, given the challenges communities are facing.
- Make sure that technology doesn’t create more problems than it solves; not all of our partners/participants will have the same access to technology.
- The difference between working in rural and urban communities is becoming more stark. Some services and/or research activities are simply no longer an option but through partnerships, innovative solutions can be developed.
August 2020

The Great Plains IDeA-CTR Network is happy to announce that our very own Community-Academic Partnership (CAP) Pilot awardee will be presenting her work in an upcoming Science Café later this month on Tuesday, August 25th at 7pm. A Science Café is an opportunity for a scientist or medical professional to communicate their work in a community setting. These events usually take place in a casual setting, such as a pub or coffee house, with topics of interest to folks in the community (due to COVID-19, this Science Café will be a virtual event broadcast via Zoom). Everyone is welcome to a typical Science Café, though you must be over 21 years of age if it takes place in a pub. The purpose is to start a conversation in plain language and in an inclusive and comfortable atmosphere for people with no science background. A question and answer period is also typically included.
Shannon Bartelt-Hunt, PhD, is the Donald R. Voelte, Jr. and Nancy A. Keegan Chair in the Department of Civil and Environmental Engineering at the University of Nebraska-Lincoln. She has a courtesy appointment in the Department of Environmental Agricultural, and Occupational Health in the College of Public Health at the University of Nebraska Medical Center. Her research focuses on contaminant fate and transport in agricultural systems, citizen science, and water reuse in agriculture.
For this event, Shannon will discuss her work involving citizen scientists and the testing of well water quality in the state of Nebraska. A State of Nebraska report found that potentially 80% of private water supply wells may exceed the drinking water standard for nitrate. In her CAP project, she engages citizen scientists to monitor ground and surface water quality for nitrate across Eastern Nebraska. In addition to improving drinking water quality for farm families, this project will engage citizens and provide science-based education and resources enabling them to be more aware of their environment and the need for healthy water supplies. Learn more about the event on the University of Nebraska State Museum – Morril Hall FACEBOOK PAGE and WEBSITE, and register for this free event HERE.
July 2020
The National IDeA-CTR group, led by our own Dr. Matthew Rizzo, has been meeting regularly to establish COVID-19 initiatives that span the clinical and translational spectrum. These initiatives include a research registry, virtual biobank, telehealth consortium, and rural health communications network. Each initiative is led by an IDeA-CTR member and includes participation from a number of the CTR programs across the country.
The research registry was established to provide a searchable database of COVID-19 patients in CTR-related states. It serves as a tool to assess outcomes and associated risks with death or complications in patients with COVID-19, as well as in patients with asymptomatic or minimally symptomatic courses. This project is in collaboration with the National Center for Advancing Translational Sciences (NCATS) and is part of an effort called the National COVID Cohort Collaboration (N3C). N3C creates an platform to systematically collect clinical, laboratory, and diagnostic data from health care provider organizations nationwide. It will harmonize the aggregated information into a standard format and make it available rapidly for research and health care providers to accelerate COVID-19 research and provide information that may improve clinical care. A demonstration of the platform can be viewed HERE.
The virtual biobank, led by the Great Plains IDeA-CTR Co-Director Dr. Howard Fox, is an electronic database of biological specimens and other related information designed to help drive COVID-19 research. Quality biosamples and associated clinical data are key to clinical and translational research. The inability to obtain adequate numbers of biospecimens limits the power of research while poor or missing metadata limits the ability to draw accurate and meaningful conclusions. More information about the COVID-19 virtual biobank can be found HERE.
The telehealth consortium has taken advantage of the unique capabilities that the IDeA-CTR Programs possess to answer the most pressing challenges and greatest opportunities for the use of telehealth to address the COVID-19 pandemic for all Americans. Both immediate and long-term challenges and opportunities that result from the current healthcare crisis will be addressed. There have been four projects identified and established to address the use of telehealth during the COVID-19 pandemic:
- The Unintended Consequences of Switching to Telehealth on Health Care Disparities
- Current State of Telemedicine and Changes Post-COVID-19
- Telemedicine in Perinatal Health in COVID and Non-COVID Patients (the focus is on women in four high-risk categories: hypertension, diabetes, substance use, and mental health concerns)
- Telemedicine in Cancer Patients (the focus is on tele-Psychiatry Oncology)
The Rural Health Communications Network facilitates two-way communication between CTR programs and state departments of health to provide rapid, evidence-based health communication to vulnerable populations for COVID-19 and future epidemics. The network plans to develop sustainable communications infrastructure with innovative technology and a “how-to” model for rural populations. As things progress, we will be sure to keep you updated because we fully intend on meeting the challenges caused by this pandemic.
June 2020

Athena Ramos, PhD, MBA, MS, CPM
In supporting community outreach activities, it is important to pay special consideration to issues that could result in health disparities. This is especially true during the COVID-19 pandemic, where members of racial and ethnic minority groups have been disproportionally affected by the disease. Several factors contribute to these disparities, including underlying health issues, inequitable access to healthcare services, and working conditions. The question remains, what is being done from an academic or community standpoint to address these inequalities?
The agricultural and meat processing industries are perfect examples of how minority groups are adversely affected by working conditions and policies during a pandemic. While surveying employees in the meatpacking industry, Athena Ramos, PhD, an assistant professor at the University of Nebraska Medical Center in the Center for Reducing Health Disparities, noted that while some of the simpler preventive measures were taken at worksites, much more could be done. Measures such as taking temperatures of workers as they enter the plant and ensuring that they wear a face mask are easier and less costly for a company to implement. Far fewer workers reported that their companies addressed systemic issues like paid sick leave, restructuring work shifts, and increasing distancing on the production line.
UNMC, which is the host institution for our network, has been one of many organizations working to address these issues. Several programs have been initiated since the start of the pandemic. For instance, Dr. Ramos and her team have been working on outreach efforts to Latino communities across the region, helping arrange virtual meetings, creating bilingual infographics, working with organizations such as the Latino Center of the Midlands to get COVID-19 information out to the public, and promoting preventive measures through Spanish-language media outlets. The Global Center for Health Securities at the University of Nebraska Medical Center has developed a growing list of playbooks, or guides, for use by public and private organizations to use to minimize the risk that COVID-19 poses to employees and the community and to reduce disruptions to business operations. This includes a playbook for meatpacking plants.
Additionally, “The MUNA Box Project” – which is led by UNMC medical students – aims to distribute information and essential resources to refugee and immigrant populations in Nebraska (also read: UNMC working to address COVID-19 health disparities). A “Period Product Drive” is collecting personal hygiene products for women at the Stephen Center and the Women’s Center for Advancement. The UNMC CoRe: COVID Relief is another student-run program “designed to connect students and community members with opportunities to assist throughout the COVID-19 outbreak.” There are many opportunities to donate, volunteer, and assist in lessening the burden of COVID-19 on some of our most vulnerable groups. The GP IDeA-CTR will continue to update the community on the current pandemic as new information becomes available.
May 2020

Our partners at the Central States Center for Agricultural Safety and Health (CS-CASH) are once again accepting registrations for their summer AgriMed course which begin in July 2020. According to the registration website, “The Agricultural Health and Safety Course for Medical and Safety Professionals is designed to examine key health and safety issues specific to rural and agricultural workers. Experts will present course material relevant to those working in health care, public health, education, and safety professions. This course is intended for professionals who work with or have an interest in agricultural health and safety including physicians, nurses, emergency medical responders, physician assistants, health educators, advanced practice nurses, Ag extension, migrant health clinicians, physical therapists, insurance specialists, veterinarians, safety professionals, and students.”
What’s exciting about this summer’s course is that it is being offered free of charge in honor of frontline healthcare workers and essential service members! Registration is still required, but participants can virtually attend the course and receive continuing education credits courtesy of its sponsors, which include CS-CASH, AgriSafe Network of Nebraska, and UNMC. Everyone who is interested in learning more about agricultural health and safety is welcome to attend.
The purpose of this course is to 1), evaluate the core elements of agricultural medicine, 2) integrate the anticipation, recognition, diagnosis, treatment, and prevention of occupational and environmental illnesses and injuries within rural and agricultural communities, and 3) learn strategies to develop sustainable agricultural occupational health and safety delivery programs within their regions. The course begins on July 14th and the registration deadline is July 7th. Learn more about the course and get registered on this website.
April 2020

Addiction comes in many forms. From substances like alcohol to doctor prescribed medications, people of all ages are capable of abusing substances to the point of addiction. Many of the efforts to prevent or reduce substance abuse and addiction are focused on younger generations. However, the prevalence of substance abuse is growing in older generations and the effects can be much more severe in this community.
Though alcohol is still the number one substance that older adults use, opioid abuse has doubled among seniors from 2002 to 2014. Many seniors deal with chronic pain and as many as 8 in 10 seniors have multiple health-related conditions. Doctors are more aware of the dangers of prescribing pain killers, but some senior citizens may have become dependent years ago and are caught in a cycle of addiction. Why?
According to SeniorLiving.org, a comprehensive directory for health information and resources for older adults, some of the reasons seniors become addicted are similar to those of younger people. Boredom, depression, and physical and/or emotional pain are some of the reasons that seniors self-medicate. Other reasons may include divorce or the loss of a loved one, isolation, loss of independence, and untreated trauma. Signs that a senior citizen may be misusing substances include evidence of increased use (e.g. empty liquor or prescription bottles), mood swings, anxiety, “doctor shopping,” and multiple prescriptions filled from different pharmacies.
With an increasingly aging population and the increasing isolation of many seniors due to the coronavirus, this issue is poised to grow. So, it is important to be aware of addiction risk factors such as a history of substance misuse, a history of anxiety or mental issues, loneliness, a spouse’s recent death, or chronic pain. Seniors in rural areas are often more at risk of opioid addiction due to fewer alternative treatments, a lack of resources and more limited educational opportunities about the potential risks of addiction. SeniorLiving.org is a great resource to learn about spotting early warning signs, finding techniques to talk about substance abuse, and discovering simple yet effective ways to prevent addiction. Learn more about substance abuse and addiction on THIS RESOURCE PAGE that they have developed.
March 2020 
By now, there is no doubt that you’ve heard much of the alarming information regarding Corona Virus 2019 (COVID-19). As health experts continue to keep us updated, many in the community have questions concerning the illness and what can be done. Fortunately, the health field is a collaborative one and many resources have been established from a variety of different organizations to answer questions and give direction that can stop the spread of the disease and flatten the curve.
To be clear the term “flatten the curve” describes the resulting difference when people use protective measures to prevent becoming ill compared to taking no protective measures at all. When enough people take preventive measures, our healthcare system is not inundated and therefore can adequately take care of those who do become ill. Actions as simple as regularly washing your hands, social distancing, and avoiding large gatherings and unnecessary outings can all help prevent becoming ill and therefore reduces the burden on our healthcare system.
Our clinical partners Nebraska Medicine and the University of Nebraska Medical Center have information online, updated in real-time, that is evidence-based and designed for those in the community. It’s important to know the symptoms of COVID-19 and who is most at risk. There is advice on how to protect yourself and others. Even instructions on how to make your own hand sanitizer. You can find all of these resources and more HERE and HERE. As always, the Centers for Disease Control and Prevent (CDC) is another great source of information concerning this outbreak. You can access those resources HERE. Community members may also be interested in viewing a very informative interview with NBA star, Stephen Curry, and National Institute of Health (NIH) official, Dr. Anthony Fauci, MD. That can be viewed HERE. Finally, if you are interested in tracking the spread of the disease, epidemiologists at Johns Hopkins University are doing just that HERE.
The Great Plains IDeA-CTR Network hopes that you stay safe during this precarious time. We advise you to follow the instructions of health experts leading the cause to flatten the curve. This outbreak will pass eventually, in the meantime we should all do what is necessary to protect ourselves and each other.
February 2020
Krista Fritson, PsyD, is a Professor in the Department of Psychology at the University of Nebraska Kearney (UNK). In addition to teaching, Dr. Fritson is on the Behavioral Health Education Center of Nebraska committee, which seeks to improve access to behavioral health in rural Nebraska. She is often consulted by community organizations including school systems and police departments regarding the wellbeing of the community and its inhabitants. She also works with the local LOSS (Local Outreach to Suicide Survivors) team, and reaches out to so many in the community who had a loved one die by suicide. For these reasons and many others, she was named Collaborator of the Year during our most recent Annual Scientific Meeting, an award voted on by the public. Watch her acceptance speech above in which she discusses the importance and benefits of collaboration.
October 2020

The annual Berggren Lecture Series is dedicated to Drs. Warren and Gretchen Berggren, long time advocates of public health and primary care approaches to address poverty and infant mortality. The Berggrens both graduated from UNMC in the late 1950s and followed their medical education with advanced degrees in Public Health from Harvard. They spent much of their careers providing medical care for the homeless in Omaha, serving as medical missionaries in the Belgian Congo (later Zaire), and developing voluntary community health worker networks to address health globally in low-income countries. Documented outcomes of their work included improve access to food, quality dietary intake, and decreases in stunted growth patterns common in low-income countries as well as developing strong health care and community partnerships that eradicated tetanus in a region in Haiti where 1 in 3 children were affected, historically, by tetanus.
The purpose of The Berggren Lecture Series is to honor the legacy of Drs. Gretchen and Warren Berggren by highlighting current partnerships between public health professionals and clinical and community organizations that (1) address the most pressing public health issues of our time, (2) study methods to move evidence for health promotion, disease prevention, and public health into typical community settings, and (3) move science forward while documenting community improvements in health and well-being.
This year, the lecture series was held virtually and featured presentations from local medical and public health experts as well as Dr. Ruth Berggren, Professor of Medicine – Infectious Disease at UT Health in San Antonio, the Director of the Center for Medical Humanities and Ethics, and daughter of Warren and Gretchen Berggren. Ruth discussed her experience caring for patients and populations in the wake of disasters and provides lessons learned in the aftermaths of recent disasters such as Hurricane Katrina, the Haiti Earthquake, and the COVID-19 pandemic. Other presenters described the importance of crisis communication, the concept of health equity and how the COVID-19 pandemic has affected health disparities in minority communities, and how we honor the legacy of the Berggrens by exploring ethical solutions to public health and primary care issues. Find and watch all the 2020 Berggren Series lectures on the UNMC College of Public Health Department of Health Promotion website.
September 2020
Conducting community-engaged research is challenging. In the midst of a pandemic, it can seem impossible. The second meeting of our Community-Engaged Research Interest Group (CEnRIG) gave us insight into the obstacles community-engaged researchers and their partners are facing including the changes experienced in different research areas and how some investigators have overcome these challenges. The purpose was to address important questions in the time of COVID-19: What do communities need from researchers right now? How can we overcome tech-related barriers with our research partners and participants? And, of course, what have been the biggest “Aha!” moments while conducting research in this pandemic? This discussion was paneled by two academic researchers and a community leader with years of experience in building partnerships. Alice Ammerman, DrPh, is a professor in the Department of Nutrition at the Gillings School of Global Public Health, and the Director of the Center for Health Promotion and Disease Prevention at UNC-Chapel Hill. Risto Rautiainen, PhD, is a Professor in the Department of Environmental, Agricultural & Occupational Health in the College of Public Health at UNMC. Doris Lassiter is the president and CEO of Doris Lassiter Consulting, LLC and has worked to address health disparities for decades, establishing programs and initiatives to lessen the burden on minority health. Some of the main takeaways from the session are great advice for folks hoping to continue their work and their relationships with communities. For instance,- Right now might not be the best time to start a new partnership; investigators should look towards formed partnerships for the time being.
- Involving the community at all stages of the project from start to finish is more important than ever, given the challenges communities are facing.
- Make sure that technology doesn’t create more problems than it solves; not all of our partners/participants will have the same access to technology.
- The difference between working in rural and urban communities is becoming more stark. Some services and/or research activities are simply no longer an option but through partnerships, innovative solutions can be developed.
August 2020

The Great Plains IDeA-CTR Network is happy to announce that our very own Community-Academic Partnership (CAP) Pilot awardee will be presenting her work in an upcoming Science Café later this month on Tuesday, August 25th at 7pm. A Science Café is an opportunity for a scientist or medical professional to communicate their work in a community setting. These events usually take place in a casual setting, such as a pub or coffee house, with topics of interest to folks in the community (due to COVID-19, this Science Café will be a virtual event broadcast via Zoom). Everyone is welcome to a typical Science Café, though you must be over 21 years of age if it takes place in a pub. The purpose is to start a conversation in plain language and in an inclusive and comfortable atmosphere for people with no science background. A question and answer period is also typically included.
Shannon Bartelt-Hunt, PhD, is the Donald R. Voelte, Jr. and Nancy A. Keegan Chair in the Department of Civil and Environmental Engineering at the University of Nebraska-Lincoln. She has a courtesy appointment in the Department of Environmental Agricultural, and Occupational Health in the College of Public Health at the University of Nebraska Medical Center. Her research focuses on contaminant fate and transport in agricultural systems, citizen science, and water reuse in agriculture.
For this event, Shannon will discuss her work involving citizen scientists and the testing of well water quality in the state of Nebraska. A State of Nebraska report found that potentially 80% of private water supply wells may exceed the drinking water standard for nitrate. In her CAP project, she engages citizen scientists to monitor ground and surface water quality for nitrate across Eastern Nebraska. In addition to improving drinking water quality for farm families, this project will engage citizens and provide science-based education and resources enabling them to be more aware of their environment and the need for healthy water supplies. Learn more about the event on the University of Nebraska State Museum – Morril Hall FACEBOOK PAGE and WEBSITE, and register for this free event HERE.
July 2020
The National IDeA-CTR group, led by our own Dr. Matthew Rizzo, has been meeting regularly to establish COVID-19 initiatives that span the clinical and translational spectrum. These initiatives include a research registry, virtual biobank, telehealth consortium, and rural health communications network. Each initiative is led by an IDeA-CTR member and includes participation from a number of the CTR programs across the country.
The research registry was established to provide a searchable database of COVID-19 patients in CTR-related states. It serves as a tool to assess outcomes and associated risks with death or complications in patients with COVID-19, as well as in patients with asymptomatic or minimally symptomatic courses. This project is in collaboration with the National Center for Advancing Translational Sciences (NCATS) and is part of an effort called the National COVID Cohort Collaboration (N3C). N3C creates an platform to systematically collect clinical, laboratory, and diagnostic data from health care provider organizations nationwide. It will harmonize the aggregated information into a standard format and make it available rapidly for research and health care providers to accelerate COVID-19 research and provide information that may improve clinical care. A demonstration of the platform can be viewed HERE.
The virtual biobank, led by the Great Plains IDeA-CTR Co-Director Dr. Howard Fox, is an electronic database of biological specimens and other related information designed to help drive COVID-19 research. Quality biosamples and associated clinical data are key to clinical and translational research. The inability to obtain adequate numbers of biospecimens limits the power of research while poor or missing metadata limits the ability to draw accurate and meaningful conclusions. More information about the COVID-19 virtual biobank can be found HERE.
The telehealth consortium has taken advantage of the unique capabilities that the IDeA-CTR Programs possess to answer the most pressing challenges and greatest opportunities for the use of telehealth to address the COVID-19 pandemic for all Americans. Both immediate and long-term challenges and opportunities that result from the current healthcare crisis will be addressed. There have been four projects identified and established to address the use of telehealth during the COVID-19 pandemic:
- The Unintended Consequences of Switching to Telehealth on Health Care Disparities
- Current State of Telemedicine and Changes Post-COVID-19
- Telemedicine in Perinatal Health in COVID and Non-COVID Patients (the focus is on women in four high-risk categories: hypertension, diabetes, substance use, and mental health concerns)
- Telemedicine in Cancer Patients (the focus is on tele-Psychiatry Oncology)
The Rural Health Communications Network facilitates two-way communication between CTR programs and state departments of health to provide rapid, evidence-based health communication to vulnerable populations for COVID-19 and future epidemics. The network plans to develop sustainable communications infrastructure with innovative technology and a “how-to” model for rural populations. As things progress, we will be sure to keep you updated because we fully intend on meeting the challenges caused by this pandemic.
June 2020

Athena Ramos, PhD, MBA, MS, CPM
In supporting community outreach activities, it is important to pay special consideration to issues that could result in health disparities. This is especially true during the COVID-19 pandemic, where members of racial and ethnic minority groups have been disproportionally affected by the disease. Several factors contribute to these disparities, including underlying health issues, inequitable access to healthcare services, and working conditions. The question remains, what is being done from an academic or community standpoint to address these inequalities?
The agricultural and meat processing industries are perfect examples of how minority groups are adversely affected by working conditions and policies during a pandemic. While surveying employees in the meatpacking industry, Athena Ramos, PhD, an assistant professor at the University of Nebraska Medical Center in the Center for Reducing Health Disparities, noted that while some of the simpler preventive measures were taken at worksites, much more could be done. Measures such as taking temperatures of workers as they enter the plant and ensuring that they wear a face mask are easier and less costly for a company to implement. Far fewer workers reported that their companies addressed systemic issues like paid sick leave, restructuring work shifts, and increasing distancing on the production line.
UNMC, which is the host institution for our network, has been one of many organizations working to address these issues. Several programs have been initiated since the start of the pandemic. For instance, Dr. Ramos and her team have been working on outreach efforts to Latino communities across the region, helping arrange virtual meetings, creating bilingual infographics, working with organizations such as the Latino Center of the Midlands to get COVID-19 information out to the public, and promoting preventive measures through Spanish-language media outlets. The Global Center for Health Securities at the University of Nebraska Medical Center has developed a growing list of playbooks, or guides, for use by public and private organizations to use to minimize the risk that COVID-19 poses to employees and the community and to reduce disruptions to business operations. This includes a playbook for meatpacking plants.
Additionally, “The MUNA Box Project” – which is led by UNMC medical students – aims to distribute information and essential resources to refugee and immigrant populations in Nebraska (also read: UNMC working to address COVID-19 health disparities). A “Period Product Drive” is collecting personal hygiene products for women at the Stephen Center and the Women’s Center for Advancement. The UNMC CoRe: COVID Relief is another student-run program “designed to connect students and community members with opportunities to assist throughout the COVID-19 outbreak.” There are many opportunities to donate, volunteer, and assist in lessening the burden of COVID-19 on some of our most vulnerable groups. The GP IDeA-CTR will continue to update the community on the current pandemic as new information becomes available.
May 2020

Our partners at the Central States Center for Agricultural Safety and Health (CS-CASH) are once again accepting registrations for their summer AgriMed course which begin in July 2020. According to the registration website, “The Agricultural Health and Safety Course for Medical and Safety Professionals is designed to examine key health and safety issues specific to rural and agricultural workers. Experts will present course material relevant to those working in health care, public health, education, and safety professions. This course is intended for professionals who work with or have an interest in agricultural health and safety including physicians, nurses, emergency medical responders, physician assistants, health educators, advanced practice nurses, Ag extension, migrant health clinicians, physical therapists, insurance specialists, veterinarians, safety professionals, and students.”
What’s exciting about this summer’s course is that it is being offered free of charge in honor of frontline healthcare workers and essential service members! Registration is still required, but participants can virtually attend the course and receive continuing education credits courtesy of its sponsors, which include CS-CASH, AgriSafe Network of Nebraska, and UNMC. Everyone who is interested in learning more about agricultural health and safety is welcome to attend.
The purpose of this course is to 1), evaluate the core elements of agricultural medicine, 2) integrate the anticipation, recognition, diagnosis, treatment, and prevention of occupational and environmental illnesses and injuries within rural and agricultural communities, and 3) learn strategies to develop sustainable agricultural occupational health and safety delivery programs within their regions. The course begins on July 14th and the registration deadline is July 7th. Learn more about the course and get registered on this website.
April 2020

Addiction comes in many forms. From substances like alcohol to doctor prescribed medications, people of all ages are capable of abusing substances to the point of addiction. Many of the efforts to prevent or reduce substance abuse and addiction are focused on younger generations. However, the prevalence of substance abuse is growing in older generations and the effects can be much more severe in this community.
Though alcohol is still the number one substance that older adults use, opioid abuse has doubled among seniors from 2002 to 2014. Many seniors deal with chronic pain and as many as 8 in 10 seniors have multiple health-related conditions. Doctors are more aware of the dangers of prescribing pain killers, but some senior citizens may have become dependent years ago and are caught in a cycle of addiction. Why?
According to SeniorLiving.org, a comprehensive directory for health information and resources for older adults, some of the reasons seniors become addicted are similar to those of younger people. Boredom, depression, and physical and/or emotional pain are some of the reasons that seniors self-medicate. Other reasons may include divorce or the loss of a loved one, isolation, loss of independence, and untreated trauma. Signs that a senior citizen may be misusing substances include evidence of increased use (e.g. empty liquor or prescription bottles), mood swings, anxiety, “doctor shopping,” and multiple prescriptions filled from different pharmacies.
With an increasingly aging population and the increasing isolation of many seniors due to the coronavirus, this issue is poised to grow. So, it is important to be aware of addiction risk factors such as a history of substance misuse, a history of anxiety or mental issues, loneliness, a spouse’s recent death, or chronic pain. Seniors in rural areas are often more at risk of opioid addiction due to fewer alternative treatments, a lack of resources and more limited educational opportunities about the potential risks of addiction. SeniorLiving.org is a great resource to learn about spotting early warning signs, finding techniques to talk about substance abuse, and discovering simple yet effective ways to prevent addiction. Learn more about substance abuse and addiction on THIS RESOURCE PAGE that they have developed.
March 2020 
By now, there is no doubt that you’ve heard much of the alarming information regarding Corona Virus 2019 (COVID-19). As health experts continue to keep us updated, many in the community have questions concerning the illness and what can be done. Fortunately, the health field is a collaborative one and many resources have been established from a variety of different organizations to answer questions and give direction that can stop the spread of the disease and flatten the curve.
To be clear the term “flatten the curve” describes the resulting difference when people use protective measures to prevent becoming ill compared to taking no protective measures at all. When enough people take preventive measures, our healthcare system is not inundated and therefore can adequately take care of those who do become ill. Actions as simple as regularly washing your hands, social distancing, and avoiding large gatherings and unnecessary outings can all help prevent becoming ill and therefore reduces the burden on our healthcare system.
Our clinical partners Nebraska Medicine and the University of Nebraska Medical Center have information online, updated in real-time, that is evidence-based and designed for those in the community. It’s important to know the symptoms of COVID-19 and who is most at risk. There is advice on how to protect yourself and others. Even instructions on how to make your own hand sanitizer. You can find all of these resources and more HERE and HERE. As always, the Centers for Disease Control and Prevent (CDC) is another great source of information concerning this outbreak. You can access those resources HERE. Community members may also be interested in viewing a very informative interview with NBA star, Stephen Curry, and National Institute of Health (NIH) official, Dr. Anthony Fauci, MD. That can be viewed HERE. Finally, if you are interested in tracking the spread of the disease, epidemiologists at Johns Hopkins University are doing just that HERE.
The Great Plains IDeA-CTR Network hopes that you stay safe during this precarious time. We advise you to follow the instructions of health experts leading the cause to flatten the curve. This outbreak will pass eventually, in the meantime we should all do what is necessary to protect ourselves and each other.
February 2020
Krista Fritson, PsyD, is a Professor in the Department of Psychology at the University of Nebraska Kearney (UNK). In addition to teaching, Dr. Fritson is on the Behavioral Health Education Center of Nebraska committee, which seeks to improve access to behavioral health in rural Nebraska. She is often consulted by community organizations including school systems and police departments regarding the wellbeing of the community and its inhabitants. She also works with the local LOSS (Local Outreach to Suicide Survivors) team, and reaches out to so many in the community who had a loved one die by suicide. For these reasons and many others, she was named Collaborator of the Year during our most recent Annual Scientific Meeting, an award voted on by the public. Watch her acceptance speech above in which she discusses the importance and benefits of collaboration.
January 2020

The purpose of the Great Plains IDeA-CTR Network’s new Engagement and Dissemination (E&D) Plan is to help researchers better understand, and communicate with, relevant patient, clinical, and community stakeholder groups. It is also intended to allow stakeholders to provide input on project relevance and improve the connection between clinical and translational research activities and the community at large. By specifying the intended audience for a research study, the goals of the study, community or stakeholder engagement strategies, and any potential deliverable products, investigators can improve the regional culture of science outside of the walls of our research institutions.
Starting with our 2020 Pilot awardees, the Community Engagement and Outreach (CEO) Core will begin meeting with researchers twice per year to discuss how they intend to engage with their respective community and disseminate information during and after the study is conducted. The CEO Core recommends engaging the community at multiple points throughout a study to collaboratively plan, implement, and interpret the study results—ultimately identifying new ways to disseminate research findings. The goal of this plan is not only to improve the methods by which researchers involve the community when conducting and communicating research, but also to ensure the sustainability of those studies. Research studies are most successful when the findings benefit the intended audience for years to come.
December 2019

Current funding for the Great Plains IDeA-CTR Network will end in 2021, but we have an opportunity to apply for ‘renewal’ funding from the National Institute of Health. If successful, the Great Plains IDeA Network will continue five more years, working to improve the health of communities by building infrastructure needed to assist researchers in advancing health and medical science.
We at the GP IDeA CTR have begun preparing the case for renewed funding of our Network. This renewal application has provided an opportunity to reflect back on our efforts over the past few years and identify our strengths and weaknesses. We had to overcome challenges that we didn’t expect but we also achieved major goals that were never anticipated when writing our initial funding application. We intend to use the lessons we’ve learned and the challenges we’ve overcome when envisioning our path forward. Much of the successful activities that we have engaged in will continue as long as they provide value to our stakeholders. But we also have big plans for the future, plans that will involve venturing into new and exciting territories.
The Community Engagement and Outreach (CEO) Core has plans for a “research incubator” designed to initiate and implement community-engaged research. This process will involve working with researchers, identifying important new lines of research, defining expected outcomes, and helping investigators design studies, write proposals, obtain funding, conduct research and disseminate results to individuals and organizations that can make an impact putting evidence-based research to practice. Additionally, our Professional Development Core has plans for an Early Career Investigator (ECI) Program, a funding mechanism which would offer smaller scholar awards to expand the number of researcher’s we help across the region. This award would focus on transitional training to faculty, structured mentoring, and some pilot money to support obtaining preliminary data. Furthermore, our Biostatistics, Epidemiology, and Research Design (BERD) Core and Biomedical Informatics and Cyberinfrastructure (BMI-CE) Core plan to collaborate to form a Comprehensive Health Data Coordinating Center which among other things will provide data analytics expertise on electronic health record (EHR) data.
We have much work to do but we are excited about the potential directions we can go. As we move forward, we will discover how we can be an even greater asset to the region. Stay tuned for updates.
November 2019

Siwei Zhao, PhD, assistant professor in the UNMC Department of Surgery, was the grand prize winner in the third annual CTR Superstar Competition, held in October by the Great Plains IDeA-CTR Network. Approximately 250 attendees came from across the country for the annual meeting, which this year focused on innovation and entrepreneurship in CTR.
In the Superstar competition, during which scientists “pitch” research ideas to a panel of judges, Dr. Zhao highlighted a project that introduced a novel ionic circuit-based ocular drug delivery device. Dr. Zhao was awarded $20,000 in pilot seed funding to expand the idea. An anonymous donor also contributed another $10,000 seed grant award, which went to the University of Nebraska-Lincoln’s Angela Dietsch, Ph.D., for her project on sensory manipulation in dysphagia recovery.
Krishan Arora, Ph.D., program director in the National Institute of General Medical Sciences Division for Research Capacity Building, gave a keynote speech highlighting resources and strategies for investigators to bring ideas from the ab to the market. Douglas Wright, M.D., Ph.D., president of the National Association of IDeA Principal Investigators, spoke on regional resources for fast tracking early stage science to market. Beverly Davidson, Ph.D., chief scientific strategy officer for Children’s Hospital of Philadelphia, discussed innovative new therapies for neurodegeneration.
The meeting was a great opportunity to showcase regional resources and success stories of innovation in CTR, community engagement, and GP IDeA-CTR leadership plans to further build infrastructure for CTR. “We were proud to host clinicians, basic and clinical scientists, community members, educators, and administrators at our meeting,” said Matthew Rizzo, M.D., chair of the UNMC Department of Neurological Sciences and Principle Investigator for the GP IDeA-CTR. “We welcomed a diverse set of ideas and backgrounds as we continued strengthening our network to build CTR and, ultimately, improve the health of individuals across our region.”
October 2019
Trey Andrews, is an Assistant Professor in the Department of Psychology in the Institute for Ethnic Studies at the University of Nebraska – Lincoln. He is also a recipient of the 2018 Great Plains IDeA CTR Scholar Award. Get more information on his study HERE.
September 2019

The Great Plains IDeA-CTR Network is hosting its 3rd Annual Scientific Meeting on October 23rd and 24th, 2019. It is yet another opportunity for the Network to showcase its resources, partnerships, and researchers. The Annual Scientific Meeting (ASM) brings together scientific investigators (spanning basic, translational and clinical work), university or collegiate educators, administrators, healthcare professionals (e.g., physicians, advanced practice providers and nurses), public health experts, and many more. Registration is free and open to the public; all are welcome including community members interested in getting involved in research.
The keynote speaker, Krishan Arora, PhD, is the Program Director in the Division for Research Capacity Building at the National Institute of General Medical Sciences (NIGMS). His presentation is entitled “From Lab to Market: Leveraging NIH SBIR/STTR, Translational and Entrepreneurial Resources.” Also speaking will be visual information design specialist, Hesham Hassan and Beverly Davidson, PhD, the Chief Scientific Strategy Officer and Professor of Pathology and Laboratory Medicine at the University of Pennsylvania.
Day one of the meeting will feature a series of breakout sessions for attendees to choose from. Each session will highlight one of the following topics: building and sustaining research teams, study sections and critiquing, evidence-based intervention repositories and comparative effectiveness research, intelligent algorithms in medicine, and accessing and using EHR data for CTR research. See the webpage dedicated to the ASM for more information on these breakout sessions.
One of the most highly anticipated activities of the event will again be the “CTR Superstar” award. The goal of this competition is to raise awareness of clinical and translational research conducted by promising scholars who are developing innovative tools and methods for medical research. The winning investigator/team will receive a $20,000 pilot grant award to catalyze cutting-edge research that may translate to a sustainable product or a larger federal grant. Applicants will present their work to a panel of experts and the winner will be announced during Day one of the meeting.
The Great Plains IDeA-CTR Network hopes you can attend what will surely be another informative and inspiring scientific meeting. You can view more information including the learning objectives and obtaining CME/CNE credits on our dedicated webpage. If you have questions, contact Amanda Fletcher. Don’t forget to register before the October 15th deadline. See you then!
August 2019
Bryant England, MD, is an Assistant Professor in the Department of Internal Medicine Division of Rheumatology at the University of Nebraska Medical Center. He is also a recipient of the 2018 Great Plains IDeA CTR Scholar Award. Get more information on his study HERE.
July 2019

Building healthy spaces is important to societal well-being. The average American spends approximately 90% of their time indoors. Noise, light, air quality, thermal comfort, layout, and ergonomics are just some examples of the indoor environmental conditions that can impact occupant health, productivity, and experience. Healthcare facilities are of particular concern due to the sensitive nature of patient populations and occupational demands on clinicians. Unfortunately, many hospitals remained plagued by various built environment issues – for example, preventable hospital acquired infections and medical errors are a leading cause of death in the U.S., noise remains a top complaint among nationally-mandated satisfaction surveys, and lost-workday injuries for hospital staff due to slips, trips, and falls is vastly greater than found in other industries.
An interdisciplinary initiative across the University of Nebraska is underway to transform the way healthcare environments are designed, constructed, maintained, and operated. The effort partners academic, medical, industry professionals, and community leaders working on demanding problems of healthcare environments. Examples of acoustic projects conducted through the initiative include linking Quiet Time in neonatal intensive care units to improved infant health, linking thousands of patient surveys to architectural and acoustic features of inpatient rooms to discern ways to improve patient satisfaction, and developing novel acoustic metrics linked to health and perception (click HERE for more information). Examples of air-quality projects include using advanced air cleaning and ventilation strategies, spatial design, and regenerative bio-reactive materials to better contain, disinfect, and remove pathogens from healthcare environments. Other example projects include aspects of light, layout, aesthetics, ergonomics, smart devices, simulation, security, and human-building interaction. Taken as a whole, the initiative ensures innovative and transformative approaches to designing, engineering, and operating the next generation of healthcare environments.
For more information, please contact Dr. Erica Ryherd, Associate Professor, Durham School of Architectural Engineering & Construction, University of Nebraska – Lincoln.
June 2019

May 2019
Elizabeth Heinrichs-Graham, PhD, is an Assistant Professor in the Department of Neurological Sciences at the University of Nebraska Medical Center. She is also a recipient of the 2018 Great Plains IDeA CTR Scholar Award. Get more information on her study HERE.April 2019

March 2019
Dr. Vijaya Bhatt, MD, is an Assistant Professor in the Department of Internal Medicine Division of Oncology & Hematology at the University of Nebraska Medical Center. He is also a recipient of the 2018 Great Plains IDeA CTR Scholar Award. Get more information on his study HERE.February 2019
Dr. Janelle Beadle, PhD, is an Assistant Professor in the Department of Gerontology at the University of Nebraska at Omaha. She is also a recipient of the 2018 Great Plains IDeA CTR Scholar Award. Get more information on her study HERE.
CLICK HERE for the study flyer.January 2019


Magnetic Resonance Imaging (MRI) Scanning is a type of scan that uses strong magnetic fields and radio waves to produce detailed images of the inside of the body. The scanner itself contains powerful magnets that can examine nearly every part of the body. The results of an MRI scan can be used to help diagnose conditions, plan treatments and assess how effective previous treatments have been. Thanks to a financial partnership between the Great Plains IDeA-CTR Network, the University of Nebraska Medical Center, and Nebraska Medicine, we now have a state-of-the-art version of the device available to us for research purposes.
UNMC Chancellor Jeff Gold, M.D., said the scanner was “truly a game changer,” adding that it will “help us unlock the mysteries of the brain and hopefully provide some answers to complex neurological problems such as Alzheimer’s disease and Parkinson’s disease, which presently don’t have any real solutions.” Until now, the Nebraska has not had such an advanced piece of equipment of this kind available to use for treatment or research.
This acquisition has opened a whole realm of research opportunities not possible before. Tony Wilson, Ph.D., director of the Magnetoencephalography Laboratory at UNMC/Nebraska Medicine stated, “This advanced imaging tool will allow investigators from around the region to examine the precise structure, function, and chemical composition of all parts of the body, but especially the brain…we know far less about the brain compared to the heart and other organs.”
This is a great asset available to not only UNMC/Nebraska Medicine but to all biomedical researchers throughout our network of institutions. The MRI scanner was installed in late 2018 and research is already being conducted. A dedication ceremony took place on January 9th, 2019. Click here to view the UNMC Newsroom article regarding the dedication ceremony.
December 2018
Jeanette Harder, PhD, is a professor in the Grace Abbott School of Social Work at the University of Nebraska at Omaha (UNO). Dr. Harder has formed more than 30 unique community partnerships through her STEPs program. Most of these are non-profit organizations and her work helps these community group to improve services and programs they offer. She was named Collaborator of the Year this year’s Annual Scientific Meeting, an award voted on by the public. Watch her inspired acceptance speech above in which she discusses the importance and benefits of collaboration.
November 2018

The fall season for us means hosting our Annual Scientific Meeting (ASM) once again. Our second meeting, hosted on October 10th and 11th, was yet another opportunity for the Great Plains IDeA-CTR Network to showcase its resources, partners, and researchers. This event brings together researchers, educators, administrators, healthcare professionals, public health experts, and many more. Over 200 people registered for the event which featured presentations about translating research across the clinical and translational spectrum, a panel to discuss study recruitment and retention, poster presentations, another highly anticipated “CTR Superstar” Competition, and an annual update regarding the resources and research supported by the network.
Team Science was the theme of this year’s two-day conference, and we were honored to host keynote speaker L. Michelle Bennett, PhD, Director of the Center for Research Strategy at the National Cancer Institute (NCI). Dr. Bennett discussed the importance of multidisciplinary teams as a strong catalyst for translating research. Her presentation, entitled “Team Science for CTR: A marathon not a Sprint,” highlighted the challenges of working within interdisciplinary teams and the characteristics that contribute to successful collaborations. This theme and Dr. Bennett’s presentation perfectly matches much of what we as a network hope to accomplish: researchers efficiently working with other researchers and community members across professions and expertise within a nurturing environment to produce better research results!
James Linder, MD, Chief Executive Officer of Nebraska Medicine, also helped us kick off the meeting. Dr. Linder stressed the importance of investing in higher learning. Dr. Linder believes that this investment is what has led to the success we have seen as a nation and has also contributed to science and the world. Loretta Jophlin, M.D., Ph.D., assistant professor in the UNMC Department of Internal Medicine, Division of Gastroenterology and Hepatology, was awarded the “CTR Superstar” Award with her proposed study intended to create a diagnostic test to differentiate non-alcoholic fatty liver diseases (NAFLD) from alcoholic fatty liver diseases (ALD). Dr. Jophlin was presented a $20,000 award which is poised to bring new scientific advances to the care of patients with liver disease. This year also featured a new Collaborator of the Year Award which recognizes and awards the time and dedication of special individuals who work to improve the lives within in their community through research. Jeanette Harder, PhD, who works at the University of Nebraska Omaha’s Grace Abbott School of Social Work, Public Affairs and Community Service earned the title this year and received her award at the ASM. Jeanette is the founder and director of the Support and Training for the Evaluation of Programs (STEPs) and has spent years working with various community and academic groups on a multitude of issues. Check out the full recap of the 2018 ASM where you can find the recorded presentations and other additional resources from the event.
October 2018
It is well known that clinical research plays a crucial role in advancing the diagnosis, treatment, and prevention of disease. Unfortunately, children are often underrepresented in clinical research, which significantly impacts the ability to provide evidence-based medical care for kids. In addition, there is often a mismatch between the locations where clinical research occurs and where disease is most prevalent. Racial and ethnic minorities, rural populations and patients of low socioeconomic status continue to be underrepresented in clinical trials and even more so among pediatric studies. Expanding our ability to perform high-quality, multi-center pediatric clinical trials that include underserved populations is essential to increase our understanding of child health, improve the generalizability of clinical trials data, as well as provide children with greater access to cutting-edge medical care.
Building on the Institutional Development Award (IDeA) program infrastructure, the National Institutes of Health (NIH) developed the IDeA States Pediatric Network (ISPN) in order to begin to address these gaps in pediatric clinical research. As a part of the NIH-funded Environmental influences on Child Health Outcomes (ECHO) project, the ISPN engages institutions from 17 states across the country who have historically received low levels of federal funding. The overall mission of the ISPN is to improve the reach of pediatric clinical trials to rural and underserved populations, and to enhance clinical trials capacity at the institutions who serve these populations. In order to accomplish this, the ISPN is currently developing pediatric clinical trials that aim to address ECHO’s five main priority areas, including upper and lower airway disease, obesity, pre-, peri-, and postnatal outcomes, neurodevelopment, and overall positive child health. Current and upcoming trials include ACT NOW, which aims to improve care of infants with Neonatal Opioid Withdrawal Syndrome, and VDORA, which will investigate the use of vitamin D supplementation in obese children with asthma.
As Nebraska’s representative in the ISPN, the Nebraska Pediatric Clinical Trials Unit (NPCTU) is backed by considerable institutional commitment and support from both the University of Nebraska Medical Center and Children’s Hospital & Medical Center. Led by Dr. Russell McCulloh, their team is actively working to engage junior investigators in ISPN-sponsored clinical trials, and to improve the overall quality of research by providing infrastructure and personnel support at all levels. In collaboration with UNMC’s Child Health Research Institute and the Pediatric Research Office, the NPCTU is looking forward to a future where all of Nebraska’s children have access to innovative research opportunities, and where more rural providers are engaged in clinical trials. They are always looking to expand our network of collaborators, so if you are interested in learning more about potential research opportunities, please feel free to reach out to our team at npctu@unmc.edu or visit our website.
September 2018
Imagine a network of institutions that collected and studied a wide array of risk factors concerning cancer development and progression. And imagine if this network could share information across borders and medical disciplines to design strategies for prevention, screening, early detection, and treatment of cancer. Now imagine if a group of collaborators actually created this network and worked to improve the efficiency of cancer research methods. Well you don’t need to imagine it, someone already did.
The integrated Cancer Repository for Cancer Research (iCaRe2) is a nexus of cancer-related information made available by and for patients, caregivers, researchers, and physicians. The iCaRe2 was created by the Fred and Pamela Buffett Cancer Center and is currently utilized by 58 institutions (81 distinct sites) from 23 U.S. states and one center in Italy. Their overall goals are to enable comprehensive studies of risk factors for cancer development and progression and to help develop novel strategies for prevention, screening, early detection and personalized treatment of cancer. How does it work? Physicians from the iCaRe2 institutions enroll eligible participants (adult cancer patients and high-risk individuals) into one of the 15 registries. iCaRe2 coordinators enter the clinical information while participants fill out the questionnaire, donate blood, and agree to make the collected data available to other collaborators. This allows researchers access to an array of cancer-related data from multiple regions as opposed to being limited to collecting data from a small pool of subjects based on a single region or an institution. Simply put: better, high-quality data leads to better, high-quality research. There is even a registry for controls (people who have not been diagnosed) to act as a comparison group.
As of October 1, 2018, data on more than 25,000 subjects (cancer patients, high-risk individuals, and normal controls) along with more than 95,000 biospecimens have been collected in the iCaRe2 registries, which include breast cancer, thyroid cancer, pancreatic cancer, and many more. The hope is that this registry will provide data to help with advancements in science, referred to as the “bench-to-bedside” approach. Anyone interested in learning more about iCaRe2 can go to their website to find more information. Patients and caregivers who are interested in learning more about iCaRe2 will want to check the For Patients page for instructions on how to sign up.

August 2018
In August, we hosted our 2nd Dissemination and Implementation (D&I) Science Workshop to help folks be successful with the dissemination and implementation aspects of their research proposals. It was held August 6th and 7th on UNMC’s campus. For our 2nd year running this workshop, we took the feedback from about 70 participants last year and determined how to improve this 2-day educational event. We updated materials covered in breakout sessions which included content for both beginners as well as more experienced D&I researchers. We also brought in new perspectives from experts at partner institutions like Kansas University Medical Center and even offered two-on-one consultations to give researchers the opportunity to discuss their proposal with D&I experts.
We were honored to host a number of returning keynote speakers including Dr. Russell Glasgow from UC Denver and Dr. Samantha Harden from Virginia Tech. New speakers included Dr. Ed Ellerbeck from KUMC who prompted attendees to consider how much evidence might be needed before submitting a D&I research proposal. Dr. Christie Befort, also from KUMC, gave some very useful context to D&I research by outlining a successful study she lead in the topic of obesity treatment in a rural primary care setting. She was also kind enough to invite a gentleman from her study who had served on the advisory board; he attested to the accomplishments that were implemented in the study.
UNMC’s own Drs. David Dzewaltowski, Paul Estabrooks, Fabio Almeida, and Tzeyu Michaud provided perspectives on different aspects of D&I science. David gave a talk on his own NIH-funded research grant which focuses on population health involving D&I science. David’s talk provided a practical example of a successful study that was further down the translational spectrum while Tzeyu discussed practical tools for assessing costs of D&I proposals. Paul delivered his usual warm welcome and discussed how to choose and apply different D&I theories to proposals. In the end, the workshop was a great opportunity to teach and learn about various elements of D&I science, both theoretical and practical, as well as a chance to network with like-minded researchers from different backgrounds and with different areas of expertise. We look forward to hosting again next year so stay tuned. Also, be sure to check out the list of presentations and resources relating to the workshop and D&I science.
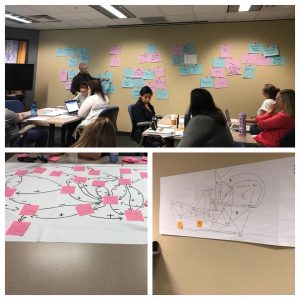
July 2018
Although 100% preventable, fetal alcohol spectrum disorder (FASD) is one of the most common birth defects in the United States. 10% of women report ever consuming alcohol during pregnancy, and recent studies indicate that up to 10% of children may have symptoms of FASD. FASD is related to a lifetime of developmental difficulties, and therefore, is an important public health issue. Although there are programs geared towards preventing FASD that are focused on reducing alcohol use or preventing unwanted pregnancy, one critical factor that is often ignored in developing these programs is the role of intimate partner violence. Women who are in violent relationships are more likely to have substance use disorders, unwanted pregnancies, and drink while they are pregnant. Some communities, such as rural areas or American Indian/Alaskan Native communities, have disproportionately high rates of FASD, as well as higher rates of intimate partner violence, and substance misuse. These areas are often challenged by allocating a limited number of resources to address a number of pressing health needs, and often lack the needed amount of resources that can dually address substance use and intimate partner violence issues for women.
The goal of Dr. Arielle Deutsch’s project is to examine community readiness and current resources within a tribal community in rural South Dakota related to reducing FASD by addressing the joint impact of intimate partner violence and substance abuse. Arielle is working with a longstanding tribal domestic violence shelter in the tribal community, to not only gather information, but also develop a coalition board that will work together to create a multi-tiered action plan for reducing substance use and intimate partner violence within the community. The overarching goal of this project is to cultivate a working relationship with advocates for Native health and wellness, who together will develop community based, high-efficacy programs for health built on current community strengths. A more immediate goal of the project is to raise awareness of the strong relationship between trauma and substance use, and the importance of addressing trauma in substance use recovery. In addition, she wants to increase community knowledge about the role of intimate partner violence and trauma in multiple aspects of child development, prenatally and postnatally. It is our hope that we can improve understanding of how intimate partner violence is not just a private issue, but a public health concern that hurts families and communities. With better knowledge, communities will be better equipped to help work on active changes and improved policies and programs geared towards reducing intimate partner violence, substance use, and improving health for current and future generations.
For more information on substance abuse and pregnancy, refer to the NIH website. You can also find resources relating to intimate partner violence at the NIH National Coalition Against Domestic Violence (NCADV) or at StrongHearts Native Helpline.

June 2018
Distress affects almost everyone diagnosed with cancer. About one-third of women with breast cancer experience significant enough distress that they feel anxious, depressed, and frequently distracted by thoughts of cancer. Many women describe a rollercoaster of emotions with both good and bad moments recurring numerous times throughout their day. These extremes of thoughts and feelings make it difficult for women with a new diagnosis of breast cancer to concentrate at work and enjoy life.
Help, however, is available. Robin Lally, PhD, MS, BA, RN, AOCN is a Professor in the College of Nursing at the University of Nebraska Medical Center who designed and created, with the help of healthcare experts and breast cancer survivors, a web-based, distress self-management program called CaringGuidance™ After Breast Cancer Diagnosis for women newly diagnosed with breast cancer. CaringGuidance™ offers women and families tools, strategies, and supportive validation for managing the thoughts, emotions and everyday distressing experiences. And, since communication with health care providers is key to receiving help for distressing cancer issues, CaringGuidance also contains a Summary Report that women may electronically create in a single page to summarize their most important concerns and facilitate communication with their clinician.
Dr. Lally was awarded a Great Plains IDeA-CTR pilot study grant to test the CaringGuidance™ Summary Report among women treated for breast cancer at the Fred & Pamela Buffett Cancer Center. Her team is interested in learning what women who use the CaringGuidance™ program for a few weeks think about how the Summary Report works, whether it is easy to use and if it contains what they find important to better communicate with their oncology clinician. They are also learning whether this helps women initiate a conversation about their thoughts and emotions during their appointment with their oncologist. This information will be used to redesign the Summary Report, making it even more useful to facilitate, communicate and help women receive distress-reducing help from their oncology clinicians. One woman has completed the study and a second woman will complete it soon. Stay tuned for the final results of this study and be sure to check out the other Pilot and Scholar projects we support.
Help, however, is available. Robin Lally, PhD, MS, BA, RN, AOCN is a Professor in the College of Nursing at the University of Nebraska Medical Center who designed and created, with the help of healthcare experts and breast cancer survivors, a web-based, distress self-management program called CaringGuidance™ After Breast Cancer Diagnosis for women newly diagnosed with breast cancer. CaringGuidance™ offers women and families tools, strategies, and supportive validation for managing the thoughts, emotions and everyday distressing experiences. And, since communication with health care providers is key to receiving help for distressing cancer issues, CaringGuidance also contains a Summary Report that women may electronically create in a single page to summarize their most important concerns and facilitate communication with their clinician.
May 2018

We hosted a Community-Based Participatory Research (CBPR) Mentoring Workshop in May which was developed to train academic researchers and community partners interested in mentoring of, and engaging community in translational research. In addition, the workshop was designed to support mentoring of academic researchers interested in community-engaged research. The workshop, sponsored by the Great Plains IDeA-CTR in conjunction with UNMC College of Public Health, Center for Reducing Health Disparities, and College of Nursing, included dynamic presentations and a panel discussion to describe and discuss foundational principles of CBPR to engage communities. Targeted to academic researchers and community partners interested in CBPR, over 30 people attended the workshop from the Midwestern region.
The event started with a welcome and introduction to the Community Engagement KCA from the co-directors Drs. Paul Estabrooks and Risto Rautiainen. They explained the aims of the KCA and the importance of engaging the local and regional community in translational research. Dr. Keyonna King – Assistant Professor at the College of Public Health, Center for Reducing Health Disparities – provided an introduction to community-engaged research and the ethical principles of CBPR. She emphasized the importance of engaging community in research and provided real world examples of successful community-academic partnered research adhering to the CBPR ethical principles.
We were honored to host our keynotes speakers, Dr. Kenneth Wells, Professor of Psychiatry and Biobehavioral Sciences at University of California Los Angeles (UCLA), Dr. Loretta Jones, activist, CEO, and Founder of Healthy African American Families II, and Ms. Felica Jones, Director of Programs at Healthy African American Families in Los Angeles, California. In the morning, Dr. Wells and Ms. Felica presented on their successful, federally funded, community-academic partnered intervention, Community Partners in Care (CPIC), to reduce disparities in depression outcomes in African Americans and Latinos in Los Angeles County. Their presentation described the successful use of CBPR to engage communities in improving depression outcomes. In the afternoon, Drs. Wells and Jones provided their perspective and recommendations for mentoring faculty, staff, and community interested in community-engaged research. They described nationally and locally successful mentoring programs they have led including but not limited to the Clinical Scholars Program, Community Faculty program at Charles R. Drew University/UCLA, and the National Center for Community Partnership Network. Rounding up the day was a panel of local and regional community-academic partners who described the formulation of their partnerships and projects to address various health or educational concerns. This was the first workshop of its kind at UNMC with a Part II follow up tentatively scheduled for the fall. You can visit our Workshop Videos page to view the sessions from our CBPR workshop or any of the workshops we’ve recently hosted. Stay tuned for information on Part II.

April 2018
 Our third Community Advisory Board (CAB) meeting was hosted this April. Members in attendance included representatives from community advocacy groups, rural health clinics, local health departments, and health systems. It was great to welcome a few new members and see the CAB in action as we discussed important and relevant issues pertaining to our collective community.
Our third Community Advisory Board (CAB) meeting was hosted this April. Members in attendance included representatives from community advocacy groups, rural health clinics, local health departments, and health systems. It was great to welcome a few new members and see the CAB in action as we discussed important and relevant issues pertaining to our collective community.
Members reviewed the overall goals and expectations of the CAB and highlighted the aspects of information dissemination and priority setting of the group. Our Health Priorities List, enacted at the previous meeting of the CAB, was addressed and we decided that the list would be looked into and possibly revised at the meeting we have planned for the fall of 2018. Members were given a full update of the GP IDeA-CTR Network including the status of our Pilot and Scholar grants as well as newly available resources such as our Collaborators Registry Dr. Rob Schwab, MD, was on hand to lay out our strategy to strengthen and expand Practice-based Research Networks (PBRNs) in the region through connections and outreach.
The “big ticket” item of this meeting was the CAB’s ranking of our Community-Academic Partnership (CAP) Program pilot applications. Our CAP Program was initiated to address real-world health issues affecting our communities through collaborations between researchers and community members. After we released our request for applications back in December 2017, we received 14 applications. Those that qualified were reviewed by our science team and the top 5 scores were presented to the CAB to be ranked in order of importance and relevance from their perspective. The proposals at the top of the list will go through an approval process and the selected project(s) will be announced soon.
We still have much work to do across the network if we intend on building the research infrastructure necessary to address the major health concerns persistent in our communities. But we are very fortunate to have access to a group of community representatives capable and willing to dedicate their time and expertise to help us with this endeavor. In the meantime, we will post CAB updates to this blog as they occur.
 Our third Community Advisory Board (CAB) meeting was hosted this April. Members in attendance included representatives from community advocacy groups, rural health clinics, local health departments, and health systems. It was great to welcome a few new members and see the CAB in action as we discussed important and relevant issues pertaining to our collective community.
Our third Community Advisory Board (CAB) meeting was hosted this April. Members in attendance included representatives from community advocacy groups, rural health clinics, local health departments, and health systems. It was great to welcome a few new members and see the CAB in action as we discussed important and relevant issues pertaining to our collective community.March 2018

As the Community Engagement and Outreach Core of the Great Plains IDeA CTR Network, we work towards bridging the gap between research efforts and community needs. We recently discovered an opportunity to improve health and wellness in communities through the development or testing of programs and interventions that are impactful and sustainable in a community setting. A funding mechanism was developed that would require a partnership between academic researchers and community groups currently working to address a health priority. What ultimately became known as our Community-Academic Partnership (CAP) Program is based on existing programs already proven successful by other CTRs and CTSIs. A funding opportunity was announced in December 2018 and by the January 31st deadline, we had received 15 applications.
Two types of awards were made available through this program. The Project award was established to generate preliminary data to assess the feasibility and acceptability of community intervention programs. The Planning award was designed to provide seed funding for investigators working to (1) develop or engage community advisory boards for project design or planning purposes or (2) engage Practice Based Research Networks to identify local priorities and begin project planning. Both awards needed to outline an existing or forming partnership between researchers and a community group and both needed to address an issue cited in our Community Advisory Board’s Health Priorities List.
All too often, programs and interventions that are based on the results of academic studies fail to take into account the implementation challenges and realities of those in the community. This issue may lessen the potentially positive impact of community-based research. On the other hand, a strong partnership between academic researchers and the community during the design, implementation, and dissemination stages of research can lead to more effective programs and reduce health disparities. Our hope is that by including the community as research partners, not just research subjects, we can advance community-engaged research and therefore improve health outcomes.

Febuary 2018

If we wish to create a better connection between research and communities, then the voice of the community needs to be present when developing and conducting community-centered projects. A major tenant of the CEO’s mission is prepare community members to not only participate but to be active research partners in the type of research that will have immediate and beneficial impact on their communities. However, any research partner who has access to participants and research data must go through the appropriate training to ensure the safety and ethical treatment of subjects and materials. Final approval for most research grant submissions involve some form of standard required training for all research partners listed on the application.
Fortunately, the Collaborative Institutional Training Initiative (CITI) Program was developed for this very reason. The CITI Program is “dedicated to promoting the public’s trust in the research enterprise by providing high quality, peer-reviewed, web-based educational courses in research, ethics, regulatory oversight, responsible conduct of research, research administration, and other topics pertinent to the interests of member organizations and individual learners.” This program, initiated in 2000, was created to provide a standard of training for the conducting of ethical research and applies to any research partner.
While academic researchers are accustomed to undergoing this type of training, community researchers may be less experienced. We have developed a simple training guide to help start the processfor any member of the community who wants to be involved in the planning, recruitment, or implementation of a community-engaged research project. And as always, we are happy to assist any community member wanting with answers to questions they might have. Our hope is that more academic researchers will reach out and engage communities in research and that those communities will be prepared to assist them when they do.

January 2018

We have found that one of the best ways to strengthen and improve research is through collaboration. Collaboration can involve two or more researchers working together to create something better than they could individually. Collaboration can also involve researchers partnering with different organizations or community groups.
Our CTR network strives to improve the research infrastructure in our region by fostering researcher-to-researcher – or researcher-to-community – collaboration. Using an interdisciplinary, cross-institutional approach can strengthen the design, execution, and results of CTR studies. To this end, we are constantly searching for new and more effective ways to bring people together.
We are fortunate to have access to a new comprehensive collaboration tool. Powered by Pure, Scopus, and Elsevier Fingerprint Engine, “Research Nebraska” was created to connect biomedical, engineering, informatics and life sciences investigators and support research collaborations. The Great Plains IDeA CTR Network has a branch of this engine specifically dedicated to our members across the region, including Nebraska, South Dakota, and North Dakota. This tool enables network members to view our registered members, research areas, ongoing projects, publications, and more. It is user friendly and frequently updated to better serve its users. You can click HERE to learn more about this collaborative tool or click HERE to go directly to our dedicated section of Research Nebraska. Whether you’re a member of a community organization hoping to find a researcher to investigate a health issue or a researcher searching for another researcher with expertise in a certain field, this comprehensive tool is an easy and effective way to find and engage other researchers in collaborative initiatives. In addition, the Community Engagement and Outreach (CEO) Core is always available for face-to-face or teleconference consultations to help bridge the gap between research and the community.
December 2017
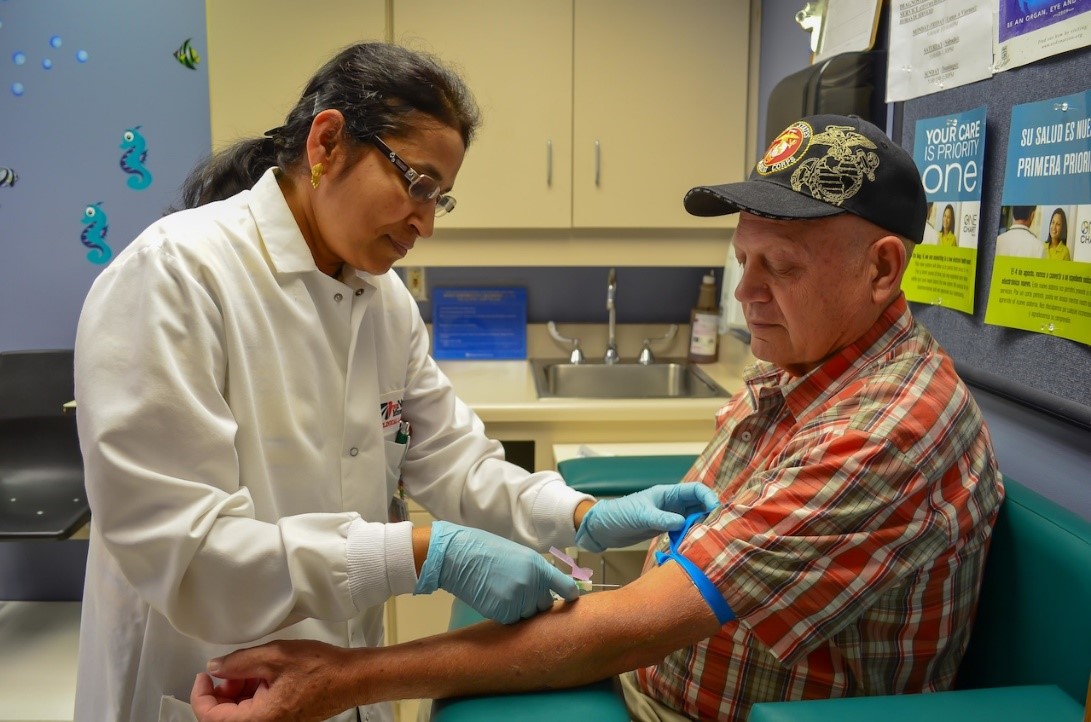
Practice-based Research Networks (PBRNs) are networks of clinicians and practices collaborating to answer health care questions that turn research findings into practice. While still treating patients as a normal clinician or practice would, PBRNs have taken the additional opportunity to explore issues related to improving patient care. Some PBRNs conduct research in specific areas such a rheumatology or mental health while others are more generalized and study quality improvement activities or access to care. Regardless of the area of study, PBRNs have integrated practice and research to address major issues in the realm of health care.
Over the last decade, the number of PBRNs in the U.S. have grown substantially to help meet the needs of an ever-changing healthcare environment. The Agency for Healthcare Research and Quality (AHRQ) is a national organization tasked with providing evidence to “make health care safer, higher quality, more accessible, equitable, and affordable.” This mission includes reporting on PBRNs, providing tools and resources, hosting events, and maintaining a registry. You can learn more about their role here. As part of our charge to improve the research infrastructure in the Great Plains region, we seek to increase the visibility of folks on the frontlines of health research and support their work. For this reason, we have developed a PBRN Directory to discover local PBRNs, find out what kind of work they do, and track their progress. And of course, there are opportunities for collaborations with these networks as well; most of our PBRNs have their contact information included in the directory. We also consult with our Community Advisory Board and our Steering Committee to develop strategies that could help expand and strengthen our local PBRNs. Further developing the networks of PBRNs would be a great opportunity to improve healthcare in our region.
November 2017

The first Annual Science Meeting for the Great Plains IDeA CTR Network was hosted recently. The two day meeting was a great opportunity for so many of us to come together to discuss the growing field of Clinical and Translational Research (CTR) as well as showcase the resources we currently have available to both communities and researchers. CTR investigators and stakeholders from a variety of organizations and professional areas were invited from all over the country with the first night of the meeting ending with a shark-tank like “CTR Superstar” competition in which Dr. David Warren won a $20,000 pilot grant award for his work to “improve memory in older adults through noninvasive brain stimulation.”
The event formally kicked off with a message from Principle Investigator, Dr. Matt Rizzo, followed by a few words from UNMC Vice Chancellor of Research, Dr. Jennifer Larson, and the Vice Chancellor of Academic Affairs, Dr. Dele Davies. It was a privilege to have keynote speaker, Dr. Christopher Austin of the National Center for Advancing Translational Science (NCATS), give insight into the direction of CTR as well as the opportunities therein. The meeting also featured a panel discussion involving community participation in research, another panel discussionrevolving around the relationship between research and community priorities, a mock review session, and interactive workshops for topics such as grant writing, community engagement, data resources, and bioinformatics. This event also gave our CTR Scholar and Pilot Award winners a chance to discuss their work including the progress they’ve made and potential future directions. We were honored that so many health professionals and researchers were able to attend. We hope that attendees found opportunities to learn and to network; establishing collaborations is something we strive for. We look forward to hosting again next year.
October 2017
Dr. Soonjo Hwang, MD is an Assistant Professor in the Department of Psychiatry at UNMC. He is also a recipient of the 2017 Great Plains IDeA CTR Scholar Award. Get more information on his study HERE.
August 2017
Daniel Rasetshwane, PhD, is the Director of the Auditory Signal Processing Laboratory at Boys Town National Research Hospital. He is also a recipient of the 2017 Great Plains IDeA CTR Scholar Award. You can find more information on his study HERE.
September 2017
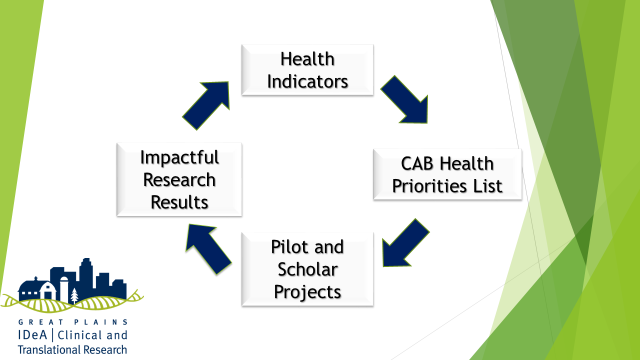
A major function of the Community Advisory Board (CAB) is to identify and prioritize regional health issues based on the members’ combined expertise and knowledge of their respective community needs. This Health Priorities List is intended to guide grant funding opportunities offered by the Great Plains IDeA CTR Network, and inform potential applicants about the research topics highlighted by our CAB members. Ideally, awarded CTR projects will discover results that will positively impact the health of the community in the near future, thus improving the major health concerns listed by CAB members.
At the inaugural meeting in March 2017, CAB members were given a presentation of major community health issues in the Great Plains IDeA CTR Center’s region. A state-by-state analysis showed that each of the Great Plains states participating in the network have certain challenges and prominent population health issues. An initial list of priorities was drafted and the list was readdressed and refined in August 2017. The list of priority health issues are as follows:
- Behavioral health
- Mental health
- Substance abuse
- Violence as a public health problem
- Obesity
- Childhood obesity
- Injury prevention
- Technologies and models to improve health access
- Connecting clinical care and community services (e.g., schools, food banks, YMCAs)
- Addressing health disparities based on social determinants, race, ethnicity, and geography
This list of issues, along with the addition of aging and age-related cognitive impairment, will be included in the request for applications for the Great Plains IDeA Pilot Grant Program. The CAB will readdress the Health Priority List every year as statistics and demographics change.
July 2017
Dr. Deepta Ghate, MD is an Assistant Professor in the Department of Ophthalmology & Visual Sciences at UNMC. She is also a recipient of the 2017 Great Plains IDeA CTR Scholar Award. Get more information on her study HERE
June 2017
One of the roles of the Community Advisory Board and the community engagement core is to help researchers prioritize research questions and plan for the movement of research into practice. Within the walls of academia and the pages of journal articles the movement of research into practice is defined as an important step on the levels of translational research.
Translational research starts from pre-clinical or human studies that test potential treatment or prevention strategies and includes testing those strategies in clinical settings under ideal conditions, then testing those strategies in typical clinics or community organizations, and finally making policy, system, and environmental changes to support those strategies benefiting whole populations of people.
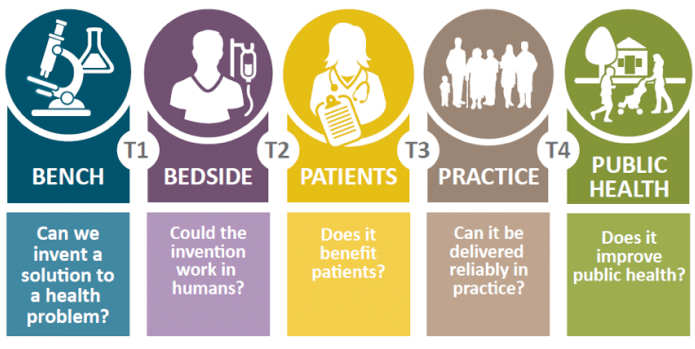
Research in the areas of pre-clinical and clinical translation, known as T1 and T2, is pretty well developed and defined, though there is still a lot of discussion about where basic science ends and translational science begins. At the other end of the spectrum, testing new treatments and preventive medicine approaches in typical clinics and communities as well as moving science into policy, system, and environmental changes—known as T3 and T4 research—is less well defined and funded. It is arguably also the type of research that can have the greatest impact on communities.
On August 14th and 15th, the Great Plains IDeA Clinical and Translational Research Network will host a workshop to help scientists develop and refine ideas for grant proposals that focus on T3 and T4 dissemination and implementation research. We have a keynote by Dr. Russ Glasgow, an international expert in implementation science and lots of local speakers with expertise and experience getting funding for this type of research. T3 and T4 research projects are intended to move science forward while also having a community impact, so if this is the type of applied work you would like to do or your community would like to engage in, come and join in for our workshop.
May 2017

Our Community Advisory Board (CAB) is a diverse group of individuals from different backgrounds and professions who are committed to assisting the Great Plains IDeA CTR Network in improving health outcomes in the region. Because CAB members understand a broad range of community health needs, they are expected to provide recommendations about research projects that are most needed to address community health issues, particularly in rural and urban underserved areas. The major CAB activities include: identifying gaps in educational and training materials that promote community health research studies, reviewing Pilot and Scholar grant applications to assess community impact, identifying ideas for potential community-engaged research projects, and encourage the expansion of practice-based research networks (PBRNs) in the region. However, the most important function of the CAB is to identify and prioritize regional health issues based on their combined expertise and knowledge of their communities. South Dakota, North Dakota, and Nebraska are all represented in our CAB and we have 15 members in total. To learn more about our CAB members, visit the Community Advisory Board page on our website.
The CAB meets twice a year and the first meeting was held on March 14th, 2017. Members were given introductory presentations by our Administration, Pilot, and Professional Development Cores. The Co-director of our Clinical Research Design, Epidemiology, and Biostatistics Core, Shinobu Watanabe-Galloway, Ph.D., also gave an in-depth presentation of the major community health issues in our region. A state-by-state analysis shows that each of the Great Plains states in the network have certain strengths and challenges which can lead to prominent health issues to their respective populations. Among the most concerning issues overall are obesity, excessive drinking, and issues related to access to care. During the meeting, CAB members discussed and identified a preliminary list of health priorities. When the CAB reconvenes in the Fall, the list of health priority issues will be finalized and used to help shape the focus of the research grants as we move forward.
April 2017
Our Community Advisory Board (CAB) is a diverse group of individuals from different backgrounds and professions who are committed to assisting the Great Plains IDeA-CTR Network in improving health outcomes in the region. Because CAB members understand a broad range of community health needs, they are expected to provide recommendations about research projects that are most needed to address community health issues, particularly in rural and urban underserved areas. The major CAB activities include: identifying gaps in educational and training materials that promote community health research studies, reviewing Pilot Grant and Scholar Award applications to assess community impact, identifying ideas for potential community-engaged research projects, and encourage the expansion of practice-based research networks (PBRNs) in the region. However, the most important function of the CAB is to identify and prioritize regional health issues based on their combined expertise and knowledge of their communities. South Dakota, North Dakota, and Nebraska are all represented in our CAB and we have 15 members in total. To learn more about our CAB members, visit the Community Advisory Board page on our website.
The CAB meets twice a year and the first meeting was held on March 14th, 2017. Members were given introductory presentations by our Administration, Pilot, and Professional Development Cores. The Co-director of our Clinical Research Design, Epidemiology, and Biostatistics Core, Shinobu Watanabe-Galloway, Ph.D., also gave an in-depth presentation of the major community health issues in our region. A state-by-state analysis shows that each of the Great Plains states in the network have certain strengths and challenges which can lead to prominent health issues to their respective populations. Among the most concerning issues overall are obesity, excessive drinking, and issues related to access to care. During the meeting, CAB members discussed and identified a preliminary list of health priorities. When the CAB reconvenes in the Fall, the list of health priority issues will be finalized and used to help shape the focus of the research grants as we move forward.
We are excited to introduce Community Conversations – a new monthly blog promoting Clinical and Translational Research (CTR). As Director of the Great Plains IDeA-CTR Community Engagement and Outreach (CEO) Core, it is my pleasure to present the first post as it gives us the opportunity to introduce ourselves and give insight into who we are and what we do. The CEO Core provides a link between CTR investigators and community partners in the region we serve. By acting as a portal between researchers and community, we hope to provide tools and information that helps to achieve our long term goal – a healthier population. In coordination with our Community Advisory Board (CAB) and participating institutions, we disseminate research findings and obtain input from the community, assisting researchers to design studies that respond to priorities identified by community members.
This monthly blog will cover topics that may be of interest to both researchers and the public. Community Conversations is an outlet for news and updates concerning the Great Plains IDeA CTR Network. Features will include upcoming community events and training opportunities, updates from CAB meetings and CTR seminars, stories from our collaborators and investigators, ongoing clinical trials, study results, grant opportunities, information about telehealth tools, and more. Anyone interested in submitting news or stories relating to CTR or community-based research opportunities should feel free to contact us.
We hope that you find this blog informative and engaging as we highlight research findings and bring the community’s voice to everyone in the Great Plains IDeA-CTR Network.